Modifiable Factors Associated with Quality of Bowel Preparation Among Hospitalized Patients Undergoing Colonoscopy
INTRODUCTION: Inadequate bowel preparation (IBP) is a common problem in hospitalized patients; however, little is known about how to prevent IBP. In a large, multihospital system, we evaluated the association between modifiable factors and IBP rate.
METHODS: We reviewed data from adult (≥18 years) inpatients undergoing colonoscopy between January 2011 and June 2017. Colonoscopies performed in the intensive care unit or lacking descriptions of bowel preparation quality were excluded. Multivariate logistic regression analysis was performed to identify factors associated with IBP. A counterfactual analysis was performed to assess the potential contribution of modifiable factors to IBP.
RESULTS: Of 8,819 patients that were included (median age of 64 years; 50.5% female), 51% had IBP. Patients with IBP stayed in the hospital one day longer than those with adequate bowel preparation (P < .001). Modifiable factors associated with IBP include opiate use within three days of colonoscopy (OR, 1.31; 95% CI, 1.18, 1.45), colonoscopy performed after 12:00 pm (OR, 1.25; 95% CI, 1.1, 1.41), and solid diet the day before colonoscopy (OR, 1.37; 95% CI, 1.18, 1.59). In the counterfactual analysis, if all patients avoided these three conditions, adjusted IBP rates were reduced by 5.6%.
CONCLUSIONS: Among hospitalized patients undergoing colonoscopy, IBP rates are high and associated with an increased length of stay. Avoiding opiates before colonoscopy, performing colonoscopy before noon, and maintaining patients on a liquid diet or nil per os might significantly reduce IBP rates.
© 2019 Society of Hospital Medicine
Outcome Measures
An internally validated natural language algorithm, using Structured Queried Language was used to search through colonoscopy reports to identify adequacy of bowel preparation. ProVation® software allows the gastroenterologist to use some terms to describe bowel preparation in a drop-down menu format. In addition to the Aronchik scale (which allows the gastroenterologist to rate bowel preparation on a five-point scale: “excellent,” “good,” “fair,” “poor,” and “inadequate”) it also allows the provider to use terms such as “adequate” or “adequate to detect polyps >5 mm” as well as “unsatisfactory.”7 Mirroring prior literature, bowel preparation quality was classified into “adequate” and “inadequate”; “good” and “excellent” on the Aronchik scale were categorized as adequate as was the term “adequate” in any form; “fair,” “poor,” or “inadequate” on the Aronchik scale were classified as inadequate as was the term “unsatisfactory.” We evaluated the hospital length of stay (LOS) as a secondary outcome measure.
Statistical Analysis
After describing the frequency of IBP, the quality of bowel preparation (adequate vs inadequate) was compared based on the predictors described above. Categorical variables were reported as frequencies with percentages and continuous variables were reported as medians with 25th-75th percentile values. The significance of the difference between the proportion or median values of those who had inadequate versus adequate bowel preparation was assessed. Two-sided chi-square analysis was used to assess the significance of differences between categorical variables and the Wilcoxon Rank-Sum test was used to assess the significance of differences between continuous variables.
Multivariate logistic regression analysis was performed to assess factors associated with hospital predictors and outcomes, after adjusting for all the aforementioned factors and clustering the effect based on the endoscopist. To evaluate the potential impact of modifiable factors on IBP, we performed counterfactual analysis, in which the observed distribution was compared to a hypothetical population in which all the modifiable risk factors were optimal.
RESULTS
Overall, 8,819 patients were included in our study population. They had a median age of 64 [53-76] years; 50.5% were female and 51% had an IBP. Patient characteristics and rates of IBP are presented in Table 1.
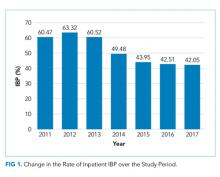
In unadjusted analyses, with regards to modifiable factors, opiate use within three days of colonoscopy was associated with a higher rate of IBP (55.4% vs 47.3%, P <.001), as was a lower volume (<4L) bowel preparation (55.3% vs 50.4%, P = .003). IBP was less frequent when colonoscopy was performed before noon vs afternoon (50.3% vs 57.4%, P < .001), and when patients were documented to receive a clear liquid diet or nil per os vs a solid diet the day prior to colonoscopy (50.3% vs 57.4%, P < .001). Overall bowel preparation quality improved over time (Figure 1). Median LOS was five [3-11] days. Patients who had IBP on their initial colonoscopy had a LOS one day longer than patients without IBP (six days vs five days, P < .001).
Multivariate Analysis
Table 2 shows the results of the multivariate analysis. The following modifiable factors were associated with IBP: opiate used within three days of the procedure (OR 1.31; 95% CI 1.8, 1.45), having the colonoscopy performed after12:00