Do Hospitals Participating in Accountable Care Organizations Discharge Patients to Higher Quality Nursing Homes?
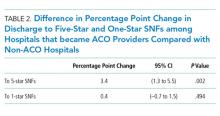
We examined whether hospitals participating in Medicare’s Shared Saving Program increased the use of highly rated skilled nursing facilities (SNFs) or decreased the use of low-rated SNFs hospital-wide after initiation of their accountable care organization (ACO) contracts compared with non-ACO hospitals. Using a difference-in-differences design, we estimated the change in the probability of discharge to 5-star and 1-star SNFs among all beneficiaries discharged from ACO-participating hospitals after the hospital initiated ACO participation. After joining an ACO, the percentage of hospital discharges going to a high-quality SNF increased by 3.4 percentage points on a base of 15.4% (95% confidence interval [CI] 1.3-5.5, P = .002) compared with non-ACO-participating hospitals. The probability of discharge from an ACO-participating hospital to low-quality SNFs did not change significantly compared with non-ACO-participating hospitals. Our findings indicate that ACO-participating hospitals were more likely to discharge patients to highly rated SNFs after they began their ACO contract but did not change the likelihood of discharge to lower rated SNFs in comparison with non-ACO hospitals.
© 2019 Society of Hospital Medicine
The probability of discharge from an ACO hospital to low-quality (one-star) SNFs did not change significantly from its baseline level of 13.5% after joining an ACO compared with non-ACO-participating hospitals (change of 0.4 percentage points, 95% CI, 0.7-1.5, P = .494).
DISCUSSION
Our findings indicate that ACO-participating hospitals were more likely to discharge patients to the highest rated SNFs after they began their ACO contract but did not change the likelihood of discharge to lower rated SNFs in comparison with non-ACO hospitals. Previous research has suggested that patients attributed to a Medicare ACO were not more likely to use high-quality SNFs. However, we examined the effect of hospital participation in an ACO, not individual beneficiaries attributed to an ACO. These contrasting results suggest that hospitals could be instituting hospital-wide changes in discharge patterns once they join an ACO and that hospital-led ACOs could be particularly well positioned to manage postdischarge care relative to physician-led ACOs. One potential limitation of this study is that ACO-participating hospitals may differ in unobservable ways from non-ACO-participating hospitals. However, using hospital fixed effects, w
Disclosures
Dr. Werner reports receiving personal fees from CarePort Health. Dr. Bain reports no conflicts. Mr. Yuan reports no conflicts. Dr. Navathe reports receiving personal fees from Navvis and Company, Navigant Inc., Lynx Medical, Indegene Inc., Sutherland Global Services, and Agathos, Inc.; personal fees and equity from NavaHealth; an honorarium from Elsevier Press, serving on the board of Integrated Services, Inc. without compensation, and grants from Hawaii Medical Service Association, Anthem Public Policy Institute, and Oscar Health, none of which are related to this manuscript.
Funding
This research was funded by R01-HS024266 by the Agency for Healthcare Research and Quality. Rachel Werner was supported in part by K24-AG047908 from the National Institute on Aging.