Recommendations on the Use of Ultrasound Guidance for Adult Abdominal Paracentesis: A Position Statement of the Society of Hospital Medicine
1. We recommend that ultrasound guidance should be used for paracentesis to reduce the risk of serious complications, the most common being bleeding.
2. We recommend that ultrasound guidance should be used to avoid attempting paracentesis in patients with an insufficient volume of intraperitoneal free fluid to drain. 3. We recommend that ultrasound guidance should be used with paracentesis to improve the success rates of the overall procedure.
4. We recommend that ultrasound should be used to assess the volume and location of intraperitoneal free fluid to guide clinical decision making of where paracentesis can be safely performed.
5. We recommend that ultrasound should be used to identify a needle insertion site based on size of the fluid collection, thickness of the abdominal wall, and proximity to abdominal organs.
6. We recommend that the needle insertion site should be evaluated using color flow Doppler ultrasound to identify and avoid abdominal wall blood vessels along the anticipated needle trajectory.
7. We recommend that a needle insertion site should be evaluated in multiple planes to ensure clearance from underlying abdominal organs and detect any abdominal wall blood vessels along the anticipated needle trajectory.
8. We recommend that a needle insertion site should be marked with ultrasound immediately before performing the procedure, and the patient should remain in the same position between marking the site and performing the procedure.
9. We recommend that using real-time ultrasound guidance for paracentesis should be considered when the fluid collection is small or difficult to access.
10. We recommend that dedicated training sessions, including didactics, supervised practice on patients, and simulation-based practice, should be used to teach novices how to perform ultrasound-guided paracentesis.
11. We recommend that simulation-based practice should be used, when available, to facilitate acquisition of the required knowledge and skills to perform ultrasound-guided paracentesis. 12. We recommend that competence in performing ultrasound-guided paracentesis should be demonstrated prior to independently performing the procedure on patients.
© 2019 Society of Hospital Medicine
METHODS
Detailed methods are described in Appendix 1. The Society of Hospital Medicine (SHM) Point-of-care Ultrasound (POCUS) Task Force was assembled to carry out this guideline development project under the direction of the SHM Board of Directors, Director of Education, and Education Committee. All expert panel members were physicians or advanced-practice providers with expertise in POCUS. Expert panel members were divided into working group members, external peer reviewers, and a methodologist, and all Task Force members were required to disclose any potential conflicts of interests (Appendix 2). The literature search was conducted in two independent phases. The first phase included literature searches conducted by the five working group members themselves. Key clinical questions and draft recommendations were then prepared, and a systematic literature search was conducted by a medical librarian based on the findings of the initial literature search and draft recommendations. The Medline, Embase, CINAHL, and Cochrane medical databases were initially searched from 1975 to October 2015. Google Scholar was also searched without limiters. An updated search was conducted from November 2015 to November 2017, search strings for which are included in Appendix 3. All article abstracts were first screened for relevance by at least two members of the working group. Full-text versions of screened articles were reviewed and articles on ultrasound guidance for paracentesis were selected. The following article types were excluded: non-English language, nonhuman, age <18 years, meeting abstracts, meeting posters, letters, and editorials. All relevant systematic reviews, meta-analyses, randomized controlled trials, and observational studies of ultrasound-guided paracentesis were screened and selected. Final article selection was based on working group consensus. The selected literature was incorporated into the draft recommendations.
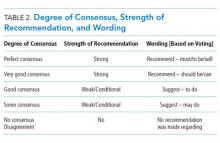
We used the RAND Appropriateness Method that required panel judgment and consensus to establish recommendations.30 The voting members of the SHM POCUS Task Force reviewed and voted on the draft recommendations considering five transforming factors: (1) problem priority and importance; (2) level of quality of evidence; (3) benefit/harm balance; (4) benefit/burden balance; and (5) certainty/concerns about preferences/equity acceptability/feasibility. Panel members participated in two rounds of electronic voting using an internet-based electronic data collection tool (Redcap™) during February 2018 and April 2018 (Appendix 4) and voting on appropriateness was conducted using a 9-point Likert scale. The three zones based on the 9-point Likert scale were inappropriate (1-3 points), uncertain (4-6 points), and appropriate (7-9 points), and the degree of consensus was assessed using the RAND algorithm (Appendix 1, Figure 1, and Table 1). Establishing a recommendation required at least 70% agreement that a recommendation was “appropriate.” A strong recommendation required 80% of the votes within one integer of the median, following RAND rules, and disagreement was defined as >30% of panelists voting outside of the zone of the median.
Recommendations were classified as strong or weak/conditional based on preset rules defining the panel’s level of consensus, which determined the wording for each recommendation (Tables 1 and 2). The revised consensus-based recommendations underwent internal and external review by POCUS experts from different subspecialties, and a final review of the guideline document was performed by members of the SHM POCUS Task Force, SHM Education Committee, and SHM Board of Directors. The SHM Board of Directors endorsed the document prior to submission to the Journal of Hospital Medicine.