Decrease in Inpatient Telemetry Utilization Through a System-Wide Electronic Health Record Change and a Multifaceted Hospitalist Intervention
BACKGROUND: Unnecessary telemetry monitoring contributes to healthcare waste.
OBJECTIVE: To evaluate the impact of 2 interventions to reduce telemetry utilization.
DESIGN, SETTING, AND PATIENTS: A 2-group retrospective, observational pre- to postintervention study of 35,871 nonintensive care unit (ICU) patients admitted to 1 academic medical center.
INTERVENTION: On the hospitalist service, we implemented a telemetry reduction intervention including education, process change, routine feedback, and a financial incentive between January 2015 and June 2015. In July 2015, a system-wide change to the telemetry ordering process was introduced.
MEASUREMENTS: The primary outcome was telemetry utilization, measured as the percentage of daily room charges for telemetry. Secondary outcomes were mortality, escalation of care, code event rate, and appropriateness of telemetry utilization. Generalized linear models were used to evaluate changes in outcomes while adjusting for patient factors.
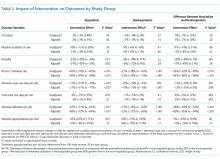
RESULTS: Among hospitalist service patients, telemetry utilization was reduced by 69% (95% confidence interval [CI], −72% to −64%; P < .001), whereas on other services the reduction was a less marked 22% (95% CI, −27% to −16%; P < .001). There were no significant increases in mortality, code event rates, or care escalation, and there was a trend toward improved utilization appropriateness.
CONCLUSION: Although electronic telemetry ordering changes can produce decreases in hospital-wide telemetry monitoring, a multifaceted intervention may lead to an even larger decline in utilization rates. Whether these changes are durable cannot be ascertained from our study.
© 2018 Society of Hospital Medicine
RESULTS
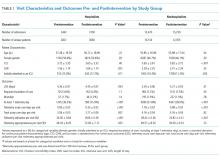
The percent of patients who had any telemetry charges decreased from 36.2% to 15.9% (P < .001) in the hospitalist group and from 31.8% to 28.0% in the nonhospitalist group (P < .001; Table 1). Rates of code events did not change over time (P = .9).
In the randomly selected sample of patients pre- and postintervention who received telemetry monitoring, there was an increase in telemetry appropriateness on the hospitalist service (46% to 72%, P = .025; Table 1). In the nonhospitalist group, appropriate telemetry utilization did not change significantly. Of the 100 randomly selected patients in the hospitalist group after the intervention who did not receive telemetry, no patient had an AHA Class I indication, and only 4 patients had a Class II indication.3,17
DISCUSSION
In this study, implementing a change in the EHR telemetry order produced reductions in telemetry days. However, when combined with a multicomponent program including education, audit and feedback, financial incentives, and changes to remove telemetry orders from admission orders sets, an even more marked improvement was seen. Neither intervention reduced LOS, increased code event rates, or increased rates of escalation of care.
Prior studies have evaluated interventions to reduce unnecessary telemetry monitoring with varying degrees of success. The most successful EHR intervention to date, from Dressler et al.,18 achieved a 70% reduction in overall telemetry use by integrating the AHA guidelines into their EHR and incorporating nursing discontinuation guidelines to ensure that telemetry discontinuation was both safe and timely. Other studies using stewardship approaches and standardized protocols have been less successful.19,20 One study utilizing a multidisciplinary approach but not including an EHR component showed modest improvements in telemetry.21
Although we are unable to differentiate the exact effect of each component of the intervention, we did note an immediate decrease in telemetry orders after removing the telemetry order from our admission order set, a trend that was magnified after the addition of broader EHR changes (Figure 1). Important additional contributors to our success seem to have been the standardization of rounds to include daily discussion of telemetry and the provision of routine feedback. We cannot discern whether other components of our program (such as the financial incentives) contributed more or less to our program, though the sum of these interventions produced an overall program that required substantial buy in and sustained focus from the hospitalist group. The importance of the hospitalist program is highlighted by the relatively large differences in improvement compared with the nonhospitalist group.
Our study has several limitations. First, the study was conducted at a single center, which may limit its generalizability. Second, the intervention was multifaceted, diminishing our ability to discern which aspects beyond the system-wide change in the telemetry order were most responsible for the observed effect among hospitalists. Third, we are unable to fully account for baseline differences in telemetry utilization between hospitalist and nonhospitalist groups. It is likely that different services utilize telemetry monitoring in different ways, and the hospitalist group may have been more aware of the existing guidelines for monitoring prior to the intervention. Furthermore, we had a limited sample size for the chart audits, which reduced the available statistical power for determining changes in the appropriateness of telemetry utilization. Additionally, because internal medicine residents rotate through various services, it is possible that the education they received on their hospitalist rotation as part of our intervention had a spillover effect in the nonhospitalist group. However, any effect should have decreased the difference between the groups. Lastly, although our postintervention time period was 1 year, we do not have data beyond that to monitor for sustainability of the results.