The Burden of Guardianship: A Matched Cohort Study
BACKGROUND: In cases where patients are unable to provide informed consent and have no surrogate decision-maker, a hospital must seek guardian appointment as a legally recognized surrogate decision-maker.
OBJECTIVE: The aim of this study was to examine the magnitudes of length of stay (LOS) beyond medical clearance and healthcare costs among patients referred for guardianship.
DESIGN, SETTING AND PATIENTS: This was a retrospective cohort study of all 61 adult inpatients in a single tertiary care hospital requiring guardianship between October 1, 2014, and September 30, 2015, matched with up to 3 controls from the same discharging services and hospitalized for at least as long as the date of clearance for referred patients.
MEASUREMENTS: The following parameters were measured using generalized estimating equations: total LOS, LOS beyond medical clearance (excess LOS), medical complications, and total charges among referred patients, and the LOS and costs were compared with those of matched controls.
RESULTS: Mean LOS for patients requiring guardianship was 31 ± 2 days, and the total charges averaged $179,243 ± 22,950. We documented 12 hospital-acquired complications in 10 (16%; 95% confidence interval [CI], 8%–28%) unique patients. Accounting for potential confounders, the process of obtaining guardianship was associated with a 37% longer total LOS (95% CI [12%-67%]; P = .002), 58% higher excess LOS (95% CI [2%-145%]; P = .04), and 23% higher total charges (95% CI [4%-46%]; P = .02).
CONCLUSION: In this single-center cohort study, the guardianship process was associated with prolonged hospital stay and higher total hospital charges even when compared with matched controls. Furthermore, one in six patients suffered from a hospital-associated complication after medical clearance.
© 2018 Society of Hospital Medicine
Covariates and Outcomes
We collected the details regarding age, gender, primary language, highest level of education, marital status, insurance status, race, date of admission, date of discharge, discharge disposition, principal diagnosis, case mix index (CMI), and discharging service from our administrative and billing data. Outcomes of interest included length of stay and total hospital charges that were collected from the same databases. We used hospital charges, rather than payments, to ensure uniformity across payers.
Chart Review
Unique to cases, a team of two medical residents (JP, RP) and a hospitalist (DR) determined the date of medical clearance and hospital-associated complications by a chart review. The date of medical clearance was then used to calculate excess length of stay, ie, the duration of stay beyond the date of medical clearance, by subtracting the time to medical clearance from the total inpatient length of stay.
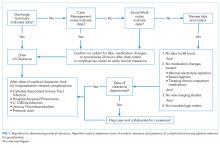
We developed a novel algorithm to determine the date of medical clearance consistently (Figure 1). We first determined whether the discharge summary indicated a clear date of medical readiness for discharge. If the discharge summary was unclear, then a case management or a social work note was used. The date of medical clearance determined by the case management or the social work note was then confirmed with clinical data. The date was confirmed if there were no significant laboratory orders and major medication changes or procedures for 24 h from the date identified. If notes were also inconclusive, then the medical clearance was determined by a review of provider order entry. Medical readiness for discharge was then defined as the first day when there were no laboratory orders for 48 h and no significant medication changes, imaging studies, or microbiologic orders.
Hospital-acquired complications were determined to be related to the guardianship process if they occurred after the date of medical stability but prior to discharge. We did not investigate hospital-acquired complications among controls. Hospital-acquired complications were defined as follows:
- Catheter-associated urinary tract infection (CAUTI): active Foley catheter order and positive urine culture that resulted in antibiotic administration.
- Hospital-acquired pneumonia (HAP): chest X-ray or computed tomography (CT) scan showing a consolidation that resulted in antibiotic administration.
- Venous thromboembolism (VTE): positive venous ultrasound or CT angiography of the chest for deep venous thrombosis (DVT) or pulmonary embolism (PE).
- Decubitus ulcer: new wound care consultation for sacral decubitus ulceration.
- Clostridium difficile (C. diff) infection: positive stool polymerase chain reaction that resulted in antibiotic administration.
The algorithm for identifying the date of clearance and the presence of complications was piloted independently by three investigators (RP, JP, DR) using a single chart review and was redesigned until a consensus was obtained. The same three investigators then independently reviewed three additional charts, including all notes, laboratory results, imaging results, and orders, with complete agreement for both date of clearance and presence of complications. Two investigators (RP, JP) then individually reviewed the remaining 57 charts. Of these, 10 were selected a priori for review by both investigators for interrater reliability, with a mean difference of 0.5 days in the estimated time to clearance and complete concordance in complications. In addition, a third investigator (DR) independently reread 5 of the 57 reviewed charts, with complete concordance in both time to clearance and presence of complications with the original readings.
Statistical Analysis
SAS 9.3 was used for all analyses (SAS Institute Inc., Cary, NC, USA).
We first examined the demographic and clinical characteristics of all 61 patients who underwent guardianship proceedings. Second, we described the primary outcomes of interest–length of stay, costs, and likelihood of complications–in this series of patients with associated 95% confidence intervals.
Third, we examined the associations between guardianship and length of stay and healthcare costs using generalized estimating equations with clustering by matched set and compound symmetry. For length of stay, we specifically assessed excess length of stay (the matching variable) to avoid immortal time bias; we also examined the total length of stay. For all regression analyses, we adjusted for the following covariates: age, gender, education, marital status, race/ethnicity, CMI, insurance status, discharging service, and principal diagnosis. To maximize normality of residuals, costs were log-transformed; length of stay beyond clearance was log-transformed after addition of 1. For both outcomes, we back-transformed the regression coefficients and presented percent change between case and control patients. All reported tests are two-sided.
RESULTS
A total of 61 guardianship cases and 118 controls were included in the analysis.