Mortality, Length of Stay, and Cost of Weekend Admissions
BACKGROUND: Apparent increase in mortality associated with being admitted to hospital on a weekend compared to weekdays has led to controversial policy changes to weekend staffing in the United Kingdom. Studies in the United States have been inconclusive and diagnosis specific, and whether to implement such changes is subject to ongoing debate.
OBJECTIVE: To compare mortality, length of stay, and cost between patients admitted on weekdays and weekends.
DESIGN: Retrospective cohort study.
SETTING: National Inpatient Sample, an administrative claims database of a 20% stratified sample of discharges from all hospitals participating in the Healthcare Cost and Utilization Project.
PATIENTS: Adult patients who were emergently admitted from 2012 to 2014.
INTERVENTION: The primary predictor was whether the admission was on a weekday or weekend.
MEASUREMENT: The primary outcome was in-hospital mortality and secondary outcomes were length of stay and cost.
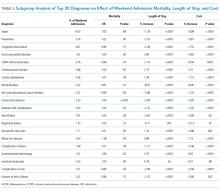
RESULTS: We included 13,505,396 patients in our study. After adjusting for demographics and disease severity, we found a small difference in inpatient mortality rates on weekends versus weekdays (odds ratio [OR] 1.029; 95% confidence interval [CI], 1.020-1.039; P < .001). There was a statistically significant but clinically small decrease in length of stay (2.24%; 95% CI, 2.16-2.33; P < .001) and cost (1.14%; 95% CI, 1.05-1.24; P < .001) of weekend admissions. A subgroup analysis of the most common weekend diagnoses showed substantial heterogeneity between diagnoses.
CONCLUSIONS: Differences in mortality of weekend admissions may be attributed to underlying differences in patient characteristics and severity of illness and is subject to large between-diagnoses heterogeneity. Increasing weekend services may not result in desired reduction in inpatient mortality rate.
© 2018 Society of Hospital Medicine
Statistical Analysis
We compared patient characteristics and other covariates between patients emergently admitted on weekends and weekdays. Continuous variables that were not normally distributed were either categorized (age, risk of mortality, and severity of illness scores) or log-transformed if right skewed (length of stay and cost). Categorical data were reported as percentages and continuous data as medians (interquartile range). We compared the inpatient mortality rate between weekend and weekday admissions by using χ2 tests. Multivariable logistic regression was used to adjust for covariates of age, gender, race, payer, income, risk of mortality and severity of illness scores, number of comorbidities, and the presence or absence of each of the 29 comorbidities available in the database to determine an adjusted odds ratio (OR), P values, and confidence intervals (CIs).
We also compared the length of stay amongst survivors and costs between weekend and weekday admissions. Multivariable linear regression was applied to the natural log of these outcome variables and the coefficients exponentiated to determine the difference in length of stay and cost of weekend admissions as compared to weekday. Covariates in the model were the same as those used for the primary outcome.
To determine if particular diagnoses had a pronounced weekend effect, the above analyses were repeated in subgroups of the top 20 most prevalent diagnoses on weekends by using the Clinical Classifications Software for ICD-9-CM diagnosis groups. For subgroup analyses, a Bonferroni correction was used, so P values of <.0025 were considered significant.
Statistical analyses were performed by using SAS version 9.4 (SAS Institute Inc, Cary, NC). All regression models were run using PROC SURVEYREG for continuous outcomes and PROC SURVEYLOGISTIC for binary outcomes to account for the sampling structure of NIS. Two-sided P values of .05 were considered significant, apart from the Bonferroni correction applied to the subgroup analysis. As this study involved publicly available deidentified data, our study was exempt from institutional board review.
RESULTS
Patient Characteristics
Mortality
The crude in-hospital mortality rate was 2.8% for patients admitted on weekends and 2.5% for patients admitted on weekdays (unadjusted OR, 1.110; 95% CI, 1.105-1.113; P < .0001). This relationship was attenuated after adjustment for demographics, severity, and comorbidities, but remained statistically significant (OR 1.029; 95% CI, 1.020-1.039; P < .0001; Table 2), which corresponds to an adjusted risk difference of 0.07% increase in mortality of weekend admissions. The OR for mortality on weekends compared to weekdays was further calculated for each of the top 20 diagnoses (Table 3). Out of all the diagnosis groups, only 1 (urinary tract infection) had a statistically significant P value after Bonferroni correction. We also looked separately at patients who were electively admitted—there was a highly significant OR of mortality of 1.67 (95% CI, 1.60-1.74). Patients classified as elective admissions were excluded for subsequent analyses.