Interventions to Reduce the Overuse of Imaging for Pulmonary Embolism: A Systematic Review
BACKGROUND: Imaging use in the diagnostic workup of pulmonary embolism (PE) has increased markedly in the last 2 decades. Low PE prevalence and diagnostic yields suggest a significant problem of overuse.
PURPOSE: The purpose of this systematic review is to summarize the evidence associated with the interventions aimed at reducing the overuse of imaging in the diagnostic workup of PE in the emergency department and hospital wards.
DATA SOURCES: PubMed, MEDLINE, Embase, and EBM Reviews from 1998 to March 28, 2017.
STUDY SELECTION: Experimental and observational studies were included. The types of interventions, their efficacy and safety, the impact on healthcare costs, the facilitators, and barriers to their implementation were assessed.
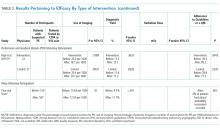
DATA SYNTHESIS: Seventeen studies were included assessing clinical decision support (CDS), educational interventions, performance and feedback reports (PFRs), and institutional policy. CDS impact was most comprehensively documented. It was associated with a reduction in imaging use, ranging from 8.3% to 25.4%, and an increase in diagnostic yield, ranging from 3.4% to 4.4%. The combined implementation of a CDS and PFR resulted in a modest but significant increase in the adherence to guidelines. Few studies appraised the safety of interventions. There was a lack of evidence concerning economic aspects, facilitators, and barriers.
CONCLUSIONS: A combined implementation of an electronic CDS and PFRs is more effective than purely educational or policy interventions, although evidence is limited. Future studies of high-methodological quality would strengthen the evidence concerning their efficacy, safety, facilitators, and barriers.
© 2018 Society of Hospital Medicine
One systematic review and meta-analysis pertaining to the impact of CDRs on CTPA use and yield was identified.29 Five of the studies it included were also included in the present review.13,16,21-23 However, its focus is different than the present one, which aims at assessing the evidence associated with the interventions being implemented to promote the use of the CDRs.29
The list of included studies appears in supplemental Appendix 2. The list of potentially relevant studies that were finally excluded is provided in supplemental Appendix 3.
Most studies (14/17) presented a before-after design, with data collection corresponding to periods preceding and following a specific intervention. Most of them are retrospective and assessed the efficacy and safety results. They were deemed of generally poor quality and were subject to many of the biases mentioned above as well as to an interaction between the intervention and its implementation context. The remaining 3 studies were experimental in design with a comparative control group.13,14,27 In 2 of these studies, a comparison was made with traditional clinical practice (no intervention).13,27 In the third, the intervention was compared with CDS only.14 The control group studies were of intermediate to very good quality and were subject to biases of performance, detection, selection, and attrition.
Table 1 summarizes the study characteristics of the included studies. The detailed methodological quality appraisal of the control group studies appears in supplemental Appendix 4.
Efficacy
CDS and PFRs
Eight of the studies appraised CDS interventions.13,16,17,19,21,22,24,28 They consisted of computer-based applications imbedded into the computerized physician order entry of the setting (ED or clinical ward of an acute care hospital), which are prompted when a physician orders an imaging exam or D-dimer test.
Educational Interventions and Policy
Seven of the interventions assessed in the included studies were educational in their essence, involving training sessions aimed at strengthening physician use of CDRs for the diagnosis of PE.15,18,20,23,25-27 Three studies observed a statistically significant impact on the
The impact of a policy fostering the use of a CDR and D-dimer was appraised in 1 study.7 This intervention translated into a significant reduction of CTPA use and a significant increase of CTPA diagnostic yield. However, only 4% of patient charts reported a clinical probability of PE, and in most cases, the type of CDR used was not mentioned.7
Safety
A minority of studies evaluated the safety of the interventions.13,18,19,23,25,27 Only 2 of these
The 2 studies involving a control group did not find significant differences between the intervention and the control groups with respect to mortality, complications because of thromboembolic and bleeding events, or any other adverse event during the 3-months’ follow-up.13,27
Jiménez et al.19 reported less than 1% mortality following the implementation of a CDS (0.7%; 95% CI, 0.2%-1.1%). In their study assessing the impact of an educational intervention, Kline et al.23 (2004) observed that none of the patients discharged with a fully negative Charlotte rule died suddenly and unexpectedly at 90-day follow-up. However, another educational intervention aimed at reducing ED patients’ radiation exposure observed a significant increase in the 90-day all-cause mortality of patients with negative CTPA, which was associated with a decline in the 90-day mortality of patients with negative ventilation/perfusion (V/Q) scanning.25
Jiménez et al.19 observed an absolute decrease of 2.5% in the incidence of symptomatic VTE events after the intervention (95% CI, 0.9%-4.6%; P < .01). The occurrence of VTE events, including PE, reached 1% in Goergen et al.18 and 3.9% in Kline et al.23 (2004) during follow-up.