Proposed In-Training Electrocardiogram Interpretation Competencies for Undergraduate and Postgraduate Trainees
Despite its importance in everyday clinical practice, the ability of physicians to interpret electrocardiograms (ECGs) is highly variable. ECG patterns are often misdiagnosed, and electrocardiographic emergencies are frequently missed, leading to adverse patient outcomes. Currently, many medical education programs lack an organized curriculum and competency assessment to ensure trainees master this essential skill. ECG patterns that were previously mentioned in literature were organized into groups from A to D based on their clinical importance and distributed among levels of training. Incremental versions of this organization were circulated among members of the International Society of Electrocardiology and the International Society of Holter and Noninvasive Electrocardiology until complete consensus was reached. We present reasonably attainable ECG interpretation competencies for undergraduate and postgraduate trainees. Previous literature suggests that methods of teaching ECG interpretation are less important and can be selected based on the available resources of each education program and student preference. The evidence clearly favors summative trainee evaluation methods, which would facilitate learning and ensure that appropriate competencies are acquired. Resources should be allocated to ensure that every trainee reaches their training milestones and should ensure that no electrocardiographic emergency (class A condition) is ever missed. We hope that these guidelines will inform medical education programs and encourage them to allocate sufficient resources and develop organized curricula. Assessments must be in place to ensure trainees acquire the level-appropriate ECG interpretation skills that are required for safe clinical practice.
© 2018 Society of Hospital Medicine
The initial draft of proposed ECG interpretation competencies was developed at Queen’s University in Ontario, Canada. A list of ECG patterns and diagnoses previously mentioned in literature was used as a starting point. From there, each item was refined and organized into 4 main categories (see Figures 1 and 2).
Class A “Common electrocardiographic emergencies” represent patterns that are frequently seen in hospitals, in which accurate interpretation of the ECG within minutes is essential for delivering care that is potentially lifesaving to the patient (eg, ST-elevation MI).
Class B “Common nonemergency patterns” represent ECG findings that are encountered daily in patients who are not acutely ill, which may impact their care in the appropriate clinical context (eg, left ventricular hypertrophy).
Class C “Uncommon electrocardiographic emergencies” represent ECG findings that are not encountered on a daily basis but can be potentially lifesaving if recognized (eg ventricular preexcitation).
Class D “Uncommon nonemergency patterns” represent findings that are uncommon but may diagnostically contribute to patient care in a clinically appropriate setting (eg, right atrial abnormality).
ECG interpretation patterns were then assigned to medical students and residents based on the specific goals of training. At the time of graduation, medical students should develop the foundation for learning ECG interpretation in residency training, provide ECG interpretation and initial management for electrocardiographic emergencies, and obtain assistance from a more senior medical professional within a clinically appropriate time frame. The training goal for a resident is to develop ECG interpretation competencies for safe independent clinical practice (Figure 1).
The final segregated ECG interpretation competencies were distributed to members of ISE and ISHNE for input, modifications, and revisions. The proposed list of competencies went through several revisions until a consensus was reached.
RESULTS
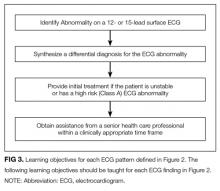
The final distribution of ECG patterns is illustrated in Figure 2. (Figure 3 defines the learning objectives for each ECG pattern defined in Figure 2.) Here, we provide a rationale for
Class A: Common Electrocardiographic Emergencies
This group contains ECG findings that require recognition within minutes to deliver potentially lifesaving care. For this reason, undergraduate medical education programs should prioritize mastering class A conditions to minimize the risk of misdiagnosis and late recognition.
Class A patterns include ST elevation MI (STEMI) and localization of territory to ensure ST-segment elevations are seen in contiguous leads.29,30 Students should learn the criteria for STEMI as per the “Universal Definition of Myocardial Infarction” and be aware of early signs of STEMI that may be seen prior to ST-segment changes, such as hyper-acute T-waves (increased amplitude and symmetrical).30
Asystole, wide complex tachycardias, and ventricular fibrillation (VF) are all crucial ECG patterns that must be identified to deliver advanced cardiac life support (ACLS) care as per the 2010 AHA Guidelines for cardiopulmonary resuscitation and emergency cardio care.31 Of note, students should understand the differential diagnosis of wide complex tachycardias and should be able to suspect VF in clinically appropriate scenarios. We included the category “unstable/symptomatic supraventricular tachycardia” to represent rapid rhythms that are supraventricular in origin, which either produce symptoms or cause impairment of vital organ function.31 In emergency situations, it may not be crucial to correctly identify the specific supraventricular rhythm to deliver ACLS care; hence, the specific supraventricular tachycardia diagnoses were included in Class B.
Finally, we believe that medical students should be able to recognize long QT, hypo/hyperkalemia, and distinguish types of atrioventricular (AV) block. Distinguishing types of AV block is important because both third degree AV block and second degree AV block Mobitz II can be life threatening and require further investigation or emergency treatment in an inpatient setting.32 Prompt recognition of long QT is crucial because it can be associated with ventricular tachyarrhythmias. This includes a polymorphic pattern characterized by the twisting of QRS peaks around the baseline (torsades des pointes), which can eventually lead to VF.