Treatment Trends and Outcomes in Healthcare-Associated Pneumonia
BACKGROUND: The American Thoracic Society and Infectious Diseases Society of America guidelines for management of healthcare-associated pneumonia (HCAP), first published in 2005, have been controversial regarding the selection of empiric broad-spectrum antibiotics, whether the criteria for HCAP predicts the likelihood of infection with multidrug resistant organisms, and whether HCAP patients have improved outcomes when treated with empiric broad-spectrum antibiotics.
METHODS: A retrospective cohort study at 488 US hospitals from July 2007 to November 2011. Patients who met criteria for HCAP were included. Guideline-concordant antibiotics were assessed based on guideline recommendations. We assessed changes in hospital rates of concordant antibiotic use over time and their correlation with outcomes.
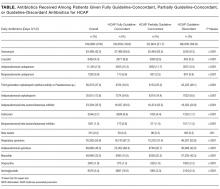
RESULTS: Among 149,963 patients with HCAP, 19.6% received fully guideline-concordant antibiotics, 21.7% received partially concordant antibiotics, and 58.9% received discordant antibiotics. Guideline concordance increased over time. Rates of fully or partially concordant antibiotics varied across hospitals (median 36.4%; interquartile range 25.8%-49.1%). Among patients who received discordant antibiotics, 81.5% were treated according to community-acquired pneumonia (CAP) guidelines. On average, the rate of guideline concordance increased by 2.2% per 6-month interval, while hospital level rates of mortality, excess length of stay, and progression to respiratory failure did not change.
CONCLUSIONS: In this large, nationally representative cohort, only 1 in 5 patients with risk factors for HCAP received treatment that was fully in accordance with guidelines, and many received CAP therapy instead. At the hospital level, increases in the use of concordant antibiotics were not associated with declines in mortality, excess length of stay, or progression to respiratory failure.
© 2017 Society of Hospital Medicine
Definitions of Guideline-Concordant and Discordant Antibiotic Therapy
The ATS and IDSA guidelines recommended the following antibiotic combinations for HCAP: an antipseudomonal cephalosporin or carbapenem or a beta-lactam/lactamase inhibitor, plus an antipseudomonal quinolone or aminoglycoside, plus an antibiotic with activity versus methicillin resistant Staphylococcus aureus (MRSA), such as vancomycin or linezolid. Based on these guidelines, we defined the receipt of fully guideline-concordant antibiotics as 2 recommended antibiotics for Pseudomonas species plus 1 for MRSA administered by the second day of admission. Partially guideline-concordant antibiotics were defined as 1 recommended antibiotic for Pseudomonas species plus 1 for MRSA by the second day of hospitalization. Guideline-discordant antibiotics were defined as all other combinations.
Statistical Analysis
Descriptive statistics on patient characteristics are presented as frequency, proportions for categorical factors, and median with interquartile range (IQR) for continuous variables for the full cohort and by treatment group, defined as fully or partially guideline-concordant antibiotic therapy or discordant therapy. Hospital rates of fully guideline-concordant treatment are presented overall and by hospital characteristics. The association of hospital characteristics with rates of fully guideline-concordant therapy were assessed by using 1-way analysis of variance tests.
To assess trends across hospitals for the association between the use of guideline-concordant therapy and mortality, progression to respiratory failure as measured by the late initiation of invasive mechanical ventilation (day 3 or later), and the length of stay among survivors, we divided the 4.5-year study period into 9 intervals of 6 months each; 292 hospitals that submitted data for all 9 time points were examined in this analysis. Based on the distribution of length of stay in the first time period, we created an indicator variable for extended length of stay with length of stay at or above the 75th percentile, defined as extended. For each hospital at each 6-month interval, we then computed risk-standardized guideline-concordant treatment (RS-treatment) rates and risk-standardized in-hospital outcome rates similar to methods used by the Centers for Medicare and Medicaid Services for public reporting.8 For each hospital at each time interval, we estimated a predicted rate of guideline-concordant treatment as the sum of predicted probabilities of guideline-concordant treatment from patient factors and the random intercept for the hospital in which they were admitted. We then calculated the expected rate of guideline-concordant treatment as the sum of expected probabilities of treatment received from patient factors only. RS-treatment was then calculated as the ratio of predicted to expected rates multiplied by the overall unadjusted mean treatment rate from all patients.9 We repeated the same modeling strategy to calculate risk-standardized outcome (RS-outcome) rates for each hospital across all time points. All models were adjusted for patient demographics and comorbidities. Similar models using administrative data have moderate discrimination for mortality.10
We then fit mixed-effects linear models with random hospital intercept and slope across time for the RS-treatment and outcome rates, respectively. From these models, we estimated the mean slope for RS-treatment and for RS-outcome over time. In addition, we estimated a slope or trend over time for each hospital for treatment and for outcome and evaluated the correlation between the treatment and outcome trends.
All analyses were performed using the Statistical Analysis System version 9.4 (SAS Institute Inc., Cary, NC) and STATA release 13 (StataCorp, LLC, College Station, Texas).