Hospital Medicine Point of Care Ultrasound Credentialing: An Example Protocol
Though the use of point-of-care ultrasound (POCUS) has increased over the last decade, formal hospital credentialing for POCUS may still be a challenge for hospitalists. This document details the Hospital Medicine Department Ultrasound Credentialing Policy from Regions Hospital, which is part of the HealthPartners organization in Saint Paul, Minnesota. National organizations from internal medicine and hospital medicine (HM) have not published recommended guidelines for POCUS credentialing. Revised guidelines for POCUS have been published by the American College of Emergency Physicians, though these are not likely intended to guide hospitalists when working with credentialing committees and medical boards. This document describes the scope of ultrasound in HM and our training, credentialing, and quality assurance program. This report is intended to be used as a guide for hospitalists as they work with their own credentialing committees and will require modification for each institution. However, the overall process described here should assist in the establishment of POCUS at various institutions.
© 2017 Society of Hospital Medicine
STEP 1: PATHWAY TO POCUS CREDENTIALING IN HM: COMPLETE MINIMAL FORMAL REQUIREMENTS
The credentialing requirements at our institution include one of the the following basic education pathways and minimal formal training:
Residency/Fellowship Based Pathway
Completed training in an Accreditation Council for Graduate Medical Education–approved program that provided opportunities for 20 hours of POCUS training with at least 6 hours of hands-on ultrasound scanning, 5 proctored limited cardiac ultrasound cases and portfolio development.
Practice Based Pathway
Completed 20 hours of POCUS continuing medical education (CME) with at least 6 hours of hands-on ultrasound scanning and has completed 5 proctored limited cardiac ultrasound cases (as part of CME).
The majority of HM providers had little formal residency training in POCUS, so a training program needed to be developed. Our training program, modeled after the American College of Chest Physicians’ CHEST certificate of completion,86 utilizes didactic training, hands-on instruction, and portfolio development that fulfills the minimal formal requirements in the practice-based pathway.
STEP 2: PATHWAY TO POCUS CREDENTIALING IN HM: COMPLETE PORTFOLIO AND FINAL ASSESSMENTS (KNOWLEDGE AND SKILLS–BASED)
After satisfactory completion of the minimal formal training, applicants need to provide documentation of a set number of cases. To aid this requirement, our HM department developed the portfolio guidelines in the Table. These are minimum requirements, and because of the varying training curves of learning,76-80 1 hospitalist may need to submit 300 files for review to meet the standards, while another may need to submit 500 files. Submissions are not accepted unless they yield high-quality video files with meticulous attention to gain, depth, and appropriate topographic planes. The portfolio development monitors hospitalists’ progression during their deliberate practice, providing objective assessments, feedback, and mentorship.81,82
A final knowledge exam with case-based image interpretation and hands-on examination is also provided. The passing score for the written examination is 85% and was based on the Angoff methodology.75 Providers who meet these requirements are then able to apply for POCUS credentialing in HM. Providers who do not pass the final assessments are required to participate in further training before they reattempt the assessments. There is uniformity in training outcomes but diversity in training time for POCUS providers.
Candidates who complete the portfolio and satisfactorily pass the final assessments are credentialed after review by the POCUS committee. Credentialed physicians are then able to perform POCUS and to integrate the findings into patient care.
MAINTENANCE OF CREDENTIALS
Documentation
After credentialing is obtained, all POCUS studies used in patient care are included in the EHR following a clearly defined workflow. The study is ordered through the EHR and is retrieved wirelessly on the ultrasound machine. After performing the ultrasound, all images are wirelessly transferred to the radiology Picture Archiving and Communication System server. Standardized text reports are used to distinguish focused POCUS from traditional diagnostic ultrasound studies. Documentation is optimized using electronic drop-down menus for documenting ultrasound findings in the EHR.
Minimum Number of Examinations
Maintenance of credentials will require that each hospitalist perform 10 documented ultrasounds per year for each cardiac and noncardiac application for which credentials are requested. If these numbers are not met, then all the studies performed during the previous year will be reviewed by the ultrasound committee, and providers will be provided with opportunities to meet the minimum benchmark (supervised scanning sessions).
Quality Assurance
Establishing scope of practice, developing curricula, and credentialing criteria are important steps toward assuring provider competence.16,17,22,74 To be confident that providers are using POCUS appropriately, there must also be a development of standards of periodic assessment that encompass both examination performance and interpretation. The objective of a QA process is to evaluate the POCUS cases for technical competence and the interpretations for clinical accuracy, and to provide feedback to improve performance of providers.
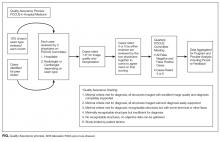
QA is maintained through the interdisciplinary POCUS committee and is described in the Figure.
After initial credentialing, continued QA of HM POCUS is done for a proportion of ongoing exams (10% as per recommendations by ACEP) to document continued competency.2 Credentialed POCUS providers perform and document their exam and interpretations. Ultrasound interpretations are reviewed by the POCUS committee (every case by 2 physicians, 1 hospitalist, and 1 radiologist or cardiologist depending on the study type) at appropriate intervals based on volume (at minimum, quarterly). A standardized review form is used to grade images and interpretations. This is the same general rubric used with the portfolio for initial credentialing. Each case is scored on a scale of 1 to 6, with 1 representing high image quality and support for diagnosis and 6 representing studies limited by patient factors. All scores rated 4 or 5 are reviewed at the larger quarterly POCUS committee meetings. For any provider scoring a 4 or 5, the ultrasound committee will recommend a focused professional practice evaluation as it pertains to POCUS. The committee will also make recommendations on a physician’s continued privileges to the department leaders.83