Dosing accuracy of direct oral anticoagulants in an academic medical center
BACKGROUND/OBJECTIVE
Direct-acting oral anticoagulants (DOACs) are increasingly used to prevent or treat thromboembolism. We conducted a study to compare how well initial DOAC prescribing for adult inpatients adhered to dosing recommendations approved by the US Food and Drug Administration (FDA).
DESIGN
Retrospective analysis.
SETTING
Single academic medical center, July 1, 2014 to June 30, 2015.
PATIENTS
508 adult inpatients.
MEASUREMENTS
DOAC prescriptions were evaluated to determine whether they met FDA-recommended dosing and administration according to patient age, weight, sex, race, kidney function, diagnoses, and concomitant medications.
RESULTS
DOACs were prescribed in 635 admissions (247 apixaban, 97 dabigatran, 291 rivaroxaban). The indication was atrial fibrillation/flutter in 465 admissions (8% with bioprostheses or valve repair), chronic deep vein thrombosis (DVT) in 67, acute DVT in 32, chronic pulmonary embolism in 23, acute pulmonary embolism in 19, DVT prevention after hip or knee surgery in 19, and non-FDA-approved indications in 10. Sixteen percent of orders for venous thromboembolic disease were for patients with active malignancy. Dosages not concordant with recommendations were prescribed for apixaban in 18% of admissions, for rivaroxaban in 14%, and for dabigatran in 7% (P = 0.04). Lower than recommended dosing was more common than higher than recommended dosing (P < 0.05). Half the deviations were continuations of outpatient dosing. Atrial fibrillation/flutter and post-hip or -knee surgery dosing deviations were more common than venous thromboembolic disease deviations (P < 0.001) but were not related to prescriber specialty.
CONCLUSIONS
DOAC prescribing recommendation deviations that can affect clinical efficacy were identified. Education and point-of-care decision support tools for improving dosing are needed, as are outcome data for patients who receive DOACs at lower than recommended dosing or for off-label indications. Journal of Hospital Medicine 2017;12:544-550. © 2017 Society of Hospital Medicine
© 2017 Society of Hospital Medicine
Accuracy of search results was confirmed by review of the first 200 patients’ records. Records were manually reviewed for encounters lacking ICD-9/10 codes and approved DOAC indications (30%) and encounters having multiple coded diagnostic indications (to identify the indication). ICD-9 codes for venous thrombosis were reviewed to differentiate acute from chronic events.
Data Analysis
The main outcome was concordance or discordance between the first DOAC prescribing order and the FDA-approved prescribing information at the time. Initial classification, performed by 2 independent reviewers (a pharmacist and a physician, or 2 pharmacists), was followed by adjudication and individual record review (by 2 independent reviewers) of all initial prescribing orders classified as discordant. A third reviewer adjudicated any disagreement. Records and notes were reviewed to identify stated or potential reasons for dosing variation and pre-admission prescriptions. Data are presented as means and standard deviations (SDs) and as raw numbers and percentages. Differences in patient characteristics by DOAC or therapeutic indication were determined by analysis of variance (ANOVA) with Bonferroni correction for post hoc comparisons. Dosing information was categorized as the same as recommended, lower than recommended, higher than recommended, or avoid drug use (drug–drug or drug–disease interaction), per FDA-approved prescribing information, and χ2 tests were used to determine whether variation in dosing occurred by individual DOAC, therapeutic indication, or prescriber specialty. Relationships between dosing variation and age or renal function were tested by ANOVA with Bonferroni correction for post hoc comparisons.
RESULTS
Patients with AF were older with lower creatinine clearance compared to patients with other diagnoses. Mean (SD) patient age was 72.1 (12.7) years for AF, 53.1 (10.9) years for chronic PE, 55.5 (14) years for acute PE, 56.4 (15.9) years for chronic DVT, 57.9 (18.4) years for acute DVT, and 61.4 (11.6) years for DVT prevention after hip or knee surgery (P < 0.0001 for all comparisons). Mean (SD) estimated creatinine clearance was 76.8 (43.5) mL/min for AF, 92.4 (44.4) mL/min for DVT prevention after hip or knee surgery, 111 (53) mL/min for chronic DVT, 118 (55) mL/min for acute DVT, 126 (60) mL/min for chronic PE, and 127 (54) mL/min for acute PE (P < 0.0001 for all comparisons). Differences between patient groups by therapeutic indication were not detected for weight, body mass index, or serum creatinine level.
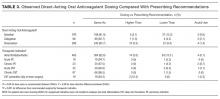
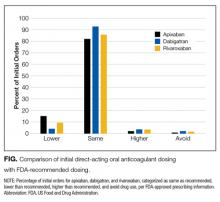
The most frequent deviation from prescribing recommendations was omission of directions to administer rivaroxaban with food—93% (248/268) of orders—but not for DVT prevention after hip or knee surgery, for which the 10-mg dose is appropriately administered without food. Doses were the same as recommended for 82% of apixaban orders, 84% of rivaroxaban orders, and 93% of initial dabigatran orders (P < 0.05 for differences; Table 3). Dosages not concordant with FDA recommendations were prescribed in 44 (18.1%) of 243 apixaban orders, 41 (14.3%) of 286 rivaroxaban orders, and 7 (7.2%) of 89 initial dabigatran orders. Lower than recommended doses were more common than higher than recommended doses (Table 3, Figure 1): 15.2% versus 2.1% of apixaban orders, 9.4% versus 3.5% of rivaroxaban orders, and 4.2% versus 1.0% of initial dabigatran orders (P < 0.05). Failure to avoid drug use (for potential drug–drug or drug–disease interactions) was uncommon (1%-2%). There were more deviations from recommended doses for patients with AF or DVT prevention after hip or knee surgery than for patients with acute or chronic PE or acute DVT (Table 3). No significant differences were detected between prescribed and recommended doses by prescriber specialty.
For apixaban, patients who were prescribed lower than recommended doses were older than those prescribed recommended doses: mean (SD), 78.1 (12.2) years versus 71 (13.6) years (P = 0.003). Seventy-six percent of those prescribed lower than recommended doses were older than 75. Prescriptions for apixaban at lower than recommended doses were continuations of prior outpatient prescriptions in 20 of 37 cases (almost half), and in 12 cases (one-fourth) antiplatelet drugs were coprescribed (aspirin in 10 cases, clopidogrel in 1, prasugrel in 1). For rivaroxaban, older age was associated with both lower than recommended dosing (P = 0.003) and higher than recommended dosing (P < 0.001). Variations from prescribing recommendations were continuations of outpatient rivaroxaban doses in about two-thirds (26 of 41; 63.4 %) with 13 receiving antiplatelet drugs. For dabigatran, 6 of 7 orders not in agreement with recommendations were continuations of outpatient dosing.
The specific equation used to estimate renal function also had the potential to lead to dosing errors. Among the 41 rivaroxaban patients categorized as receiving doses discordant with recommendations, 8 would have had an inappropriate DOAC dose if eGFR were used instead of eCrCL as recommended. No relationships were detected for other patient variables/measures and dosing deviations from recommendations.