Rates, predictors and variability of interhospital transfers: A national evaluation
Importance
Interhospital transfer (IHT) remains a largely unstudied process of care.
Objective
To determine the nationwide frequency of, patient and hospital-level predictors of, and hospital variability in IHT.
Design
Cross-sectional study.
Setting
Centers for Medicare and Medicaid 2013 100% Master Beneficiary Summary and Inpatient claims files merged with 2013 American Hospital Association data.
Patients
Beneficiaries ≥65 years and older enrolled in Medicare A and B, with an acute care hospitalization claim in 2013.
Exposures
Patient and hospital characteristics of transferred and nontransferred patients.
Measurements
Frequency of interhospital transfers (IHT); adjusted odds of transfer of each patient and each hospital characteristic; and variability in hospital transfer rates.
Results
Of 6.6 million eligible beneficiaries with an acute care hospitalization, 101,507 (1.5%) underwent IHT. Selected characteristics associated with greater adjusted odds of transfer included: patient age 74-85 years (odds ratio [OR], 2.38 compared with 65-74 years; 95% confidence intervals [CI], 2.33-2.43); nonblack race (OR, 1.17; 95% CI, 1.13-1.20); higher comorbidity (OR, 1.37; 95% CI, 1.36-1.37); lower diagnosis-related group–weight (OR, 2.02; 95% CI, 1.95-2.09); fewer recent hospitalizations (OR, 1.87; 95% CI, 1.79-1.95); and hospitalization in the Northeast (OR, 1.40; 95% CI, 1.27-1.55). Higher case mix index of the hospital was associated with a lower adjusted odds of transfer (OR, 0.36; 95% CI, 0.30-0.45). Variability in hospital transfer rates remained significant after adjustment for patient and hospital characteristics (variance 0.28, P = 0.01).
Conclusions
In this nationally representative evaluation, we found that a sizable number of patients undergo IHT. We identified both expected and unexpected patient and hospital-level predictors of IHT, as well as unexplained variability in hospital transfer rates, suggesting lack of standardization of this complex care transition. Our study highlights further investigative avenues to help guide best practices in IHT. Journal of Hospital Medicine 2017;12:435-442. © 2017 Society of Hospital Medicine
© 2017 Society of Hospital Medicine
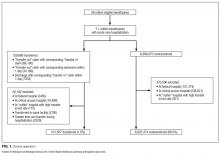
Beneficiaries were eligible for inclusion if they were 65 years or older, continuously enrolled in Medicare A and B, with an acute care hospitalization claim in 2013, excluding Medicare managed care and end-stage renal disease (ESRD) beneficiaries. We additionally excluded beneficiaries hospitalized at federal or nonacute care hospitals, or critical access hospitals given their mission to stabilize and transfer patients to referral hospitals.20
Transferred patients were defined as: (1) beneficiaries with a “transfer out” claim and a corresponding “transfer in” claim at a different hospital; as well as (2) beneficiaries with a “transfer out” claim and a corresponding date of admission to another hospital within 1 day following the date of claim; and (3) beneficiaries with a “transfer in” claim and a corresponding date of discharge from another hospital within 1 day preceding the date of claim. Beneficiaries transferred to the same hospital, or cared for at hospitals with “outlier” transfer in rates equal to 100% or transfer out rates greater than 35%, were excluded from analysis given the suggestion of nonstandard claims practices. Beneficiaries with greater than 1 transfer within the same hospitalization were additionally excluded.
Patient Characteristics
Patient characteristics were obtained from the CMS data files and included: demographics (age, sex, race); DRG-weight, categorized into quartiles; primary diagnosis for the index hospitalization using ICD-9 codes; patient comorbidity using ICD-9 codes compiled into a CMS-Hierarchical Condition Category (HCC) risk score;21 presence of Medicaid co-insurance; number of hospitalizations in the past 12 months, categorized into 0, 1, 2-3, and 4 or more; season, defined as calendar quarters; and median income per household by census tract. These characteristics were chosen a priori given expert opinion in combination with prior research demonstrating association with IHT.11,22
Hospital Characteristics
Hospital characteristics were obtained from AHA data files and included hospitals’ size, categorized into small, medium, and large (less than 100, 100 to 399, 400 or more beds); geographic location; ownership; teaching status; setting (urban vs. rural); case mix index (CMI) for all patients cared for at the hospital; and presence of selected specialty services, including certified trauma center, medical intensive care unit, cardiac intensive care unit, cardiac surgery services, adult interventional cardiac catheterization, adult cardiac electrophysiology, and composite score of presence of 55 other specialty services (complete list in Appendix A). All characteristics were chosen a priori given expert opinion or relationship of characteristics with IHT, and prior research utilizing AHA data.23-24
Analysis
Descriptive statistics were used to evaluate the frequency of IHT, characteristics of transferred patients, and number of days to transfer. Patient and hospital characteristics of transferred vs. nontransferred patients were compared using chi-square analyses.
To analyze the effects of each patient and hospital characteristic on the odds of transfer, we used logistic regression models incorporating all patient and hospital characteristics, accounting for fixed effects for diagnosis, and utilizing generalized estimating equations (the GENMOD procedure in SAS statistical software, v 9.4; SAS Institute Inc., Cary, North Carolina) to account for the clustering of patients within hospitals.25 Indicator variables were created for missing covariate data and included in analyses when missing data accounted for greater than 10% of the total cohort.
To measure the variability in transfer rates between hospitals, we used a sequence of random effects logistic regression models. We first ran a model with no covariates, representing the unadjusted differences in transfer rates between hospitals. We then added patient characteristics to see if the unadjusted differences in IHT rates were explained by differences in patient characteristics between hospitals. Lastly, we added hospital characteristics to determine if these explained the remaining differences in transfer rates. Each of the 3 models provided a measure of between-hospital variability, reflecting the degree to which IHT rates differed between hospitals. Additionally, we used the intercept from the unadjusted model and the measure of between-hospital variability from each model to calculate the 95% confidence intervals, illustrating the range of IHT rates spanning 95% of all hospitals. We used those same numbers to calculate the 25th and 75th percentiles, illustrating the range of IHT rates for the middle half of hospitals.
RESULTS
Among 28 million eligible beneficiaries, 6.6 million had an acute care hospitalization to nonfederal, noncritical access hospitals, and 107,741 met our defined criteria for IHT. An additional 3790 beneficiaries were excluded for being transferred to the same facility, 416 beneficiaries (115 transferred, 301 nontransferred) were excluded as they were cared for at 1 of the 11 hospitals with “outlier” transfer in/out rates, and 2329 were excluded because they had more than 1 transfer during hospitalization. Thus, the final cohort consisted of 101,507 transferred (1.5%) and 6,625,474 nontransferred beneficiaries (Figure 1). Of the 101,507 transferred beneficiaries, 2799 (2.8%) were included more than once (ie, experienced more than 1 IHT on separate hospitalizations throughout the study period; the vast majority of these had 2 separate hospitalizations resulting in IHT). Characteristics of transferred and nontransferred beneficiaries are shown (Table 1).