Planning and designing the Improving Addiction Care Team (IMPACT) for hospitalized adults with substance use disorder
People with substance use disorders (SUD) have high rates of hospitalization and readmission, long lengths of stay, and skyrocketing healthcare costs. Yet, models for improving care are extremely limited. We performed a needs assessment and then convened academic and community partners, including a hospital, community SUD organizations, and Medicaid accountable care organizations, to design a care model for medically complex hospitalized patients with SUD. Needs assessment showed that 58% to 67% of participants who reported active substance use said they were interested in cutting back or quitting. Many reported interest in medication for addiction treatment (MAT). Participants had high rates of costly readmissions and longer than expected length of stay. Community stakeholders identified long wait times and lack of resources for medically complex patients as key barriers. We developed the Improving Addiction Care Team (IMPACT), which includes an inpatient addiction medicine consultation service, rapid-access pathways to posthospital SUD treatment, and a medically enhanced residential care model that integrates antibiotic infusion and residential addiction care. We developed a business case and secured funding from Medicaid and hospital payers. IMPACT provides one pathway for hospitals, payers, and communities to collaboratively address the SUD epidemic. Journal of Hospital Medicine 2017;12:339-342. © 2017 Society of Hospital Medicine
© 2017 Society of Hospital Medicine
Partner Engagement
We identified community partners with which we had an individual or organizational relationship and a common interest and potential for collaboration. All invited partners agreed to attend initial meetings. We convened leadership and frontline staff across partners. OHSU staff included hospital nursing and social work leaders; infectious disease, hospitalist, and addiction physicians; and health services researchers. Community organizations included Central City Concern (CCC), a community organization serving people facing homelessness and addiction; CODA, Inc., a nonprofit SUD treatment agency; and Coram/CVS infusion pharmacy.
Collectively, we reviewed needs assessment findings and examples from the literature7-9 to develop strategies to address patient and system needs. We used patient narratives to foster alignment and prioritized areas in which integration could improve quality and costs. We assumed we would petition OHSU and/or Medicaid CCOs to finance efforts and saved potentially challenging budget discussions for later, when partnerships would be more developed. Our task force attended more than 3 large-group meetings and numerous small-group meetings to develop IMPACT.
RESULTS
Needs Assessment
Between September 2014 and April 2015, a research assistant approached 326 patients. Of these, 235 (72%) met study inclusion criteria, and 185 (78%) agreed to participate (Table 1). Of people who reported any substance use within the preceding 3 months, 58% of alcohol users and 67% of drug users said they were interested in cutting back or quitting. Fifty-four percent of participants with moderate- to high-risk opioid use and 16% with moderate- to high-risk alcohol use reported strong interest in MAT. In qualitative interviews, participants described inadequately treated withdrawal, the importance of trust and choice, and long wait times as a barriers to entering treatment after hospital discharge.20
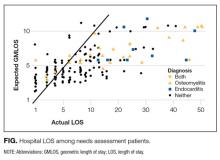
Administrative data revealed high rates of hospital readmissions and longer than expected LOS (Figure). Mean LOS was 10.26 days—4 days more than medicine patients’. Mean LOS was high among participants who required long-term IV antibiotics, particularly those with endocarditis or osteomyelitis (21.75 days; range, 1.00-51.00 days). We excluded one outlier with a 116-day hospitalization.
Intervention Design
Mapping needs to intervention components. We mapped needs assessment findings to 3 main IMPACT components: inpatient addiction medicine consultation service, pathways to posthospital SUD treatment, and medically enhanced residential treatment (MERT) (Table 2).
Inpatient addiction medicine consultation service. We developed this service to address patients’ report of high readiness to change and interest in starting MAT in the hospital. Community partners highlighted the need for peers to increase engagement and trust. Therefore, we included a physician, a social worker, and two peers on our team. The inpatient service engages patients, advises on withdrawal and pain, performs SUD assessments, initiates MAT, and provides counseling and treatment.
Pathways to posthospital SUD treatment. As pathways from hospital to community SUD treatment were lacking, and long administrative wait times limited access to community treatment, we employed “in-reach” liaisons—community SUD treatment staff who perform in-hospital assessments to triage and coordinate care across systems. Given that patients value having treatment choices, we linked pathways to an array of MAT and abstinence-based treatments, including office-based, intensive outpatient and residential levels of care. For patients who live outside the Portland area, we developed relationships with rural stakeholders and engaged the help of the Oregon State Opioid Authority in introducing our program to SUD treatment providers around the state.
Medically Enhanced Residential Treatment (MERT). In many cases where patients required prolonged courses of IV antibiotics, hospital stays were longer for two reasons: At-home central-line self-administration of antibiotics was deemed unsafe, and patients were denied admission to a skilled nursing facility due to history of substance use. These long LOS create an opportunity to initiate and engage patients in treatment, and to render savings by shifting care to a residential addiction treatment setting that can accommodate IV antibiotic administration and MAT. We increased residential staffing and collaborated with a home infusion pharmacy to administer daily infusions on site.
Funding the Intervention
We used administrative data to estimate potential savings and tailored a business case to CCO and hospital payers. The CCO business case centered on hospitalization as an opportunity to engage out-of-treatment adults and potentially reduce high-cost readmissions by managing physical and behavioral health needs. Working within budgeting time lines, we used data from the first 165 participants. These participants had 137 readmissions over a mean observation period of 4.5 months. Mean charge per readmission was $31,157 (range, $699-$206,596) and was highest for people with endocarditis (mean, $55,493; range, $23,204-$145,066) and osteomyelitis (mean, $68,774; range, $29,359-$124,481). We estimated that a 10% reduction in 6-month readmissions could avoid $674,863 in charges.