High prevalence of inappropriate benzodiazepine and sedative hypnotic prescriptions among hospitalized older adults
BACKGROUND
Benzodiazepines and sedative hypnotics are commonly used to treat insomnia and agitation in older adults despite significant risk. A clear understanding of the extent of the problem and its contributors is required to implement effective interventions.
OBJECTIVE
To determine the proportion of hospitalized older adults who are inappropriately prescribed benzodiazepines or sedative hypnotics, and to identify patient and prescriber factors associated with increased prescriptions.
DESIGN
Single-center retrospective observational study.
SETTING
Urban academic medical center.
PARTICIPANTS
Medical-surgical inpatients aged 65 or older who were newly prescribed a benzodiazepine or zopiclone.
MEASUREMENTS
Our primary outcome was the proportion of patients who were prescribed a potentially inappropriate benzodiazepine or sedative hypnotic. Potentially inappropriate indications included new prescriptions for insomnia or agitation/anxiety. We used a multivariable random-intercept logistic regression model to identify patient- and prescriber-level variables that were associated with potentially inappropriate prescriptions.
RESULTS
Of 1308 patients, 208 (15.9%) received a potentially inappropriate prescription. The majority of prescriptions, 254 (77.4%), were potentially inappropriate. Of these, most were prescribed for insomnia (222; 87.4%) and during overnight hours (159; 62.3%). Admission to a surgical or specialty service was associated with significantly increased odds of potentially inappropriate prescription compared to the general internal medicine service (odds ratio [OR], 6.61; 95% confidence interval [CI], 2.70-16.17). Prescription by an attending physician or fellow was associated with significantly fewer prescriptions compared to first-year trainees (OR, 0.28; 95% CI, 0.08-0.93). Nighttime prescriptions did not reach significance in initial bivariate analyses but were associated with increased odds of potentially inappropriate prescription in our regression model (OR, 4.48; 95% CI, 2.21-9.06).
CONCLUSIONS
The majority of newly prescribed benzodiazepines and sedative hypnotics were potentially inappropriate and were primarily prescribed as sleep aids. Future interventions should focus on the development of safe sleep protocols and education targeted at first-year trainees. Journal of Hospital Medicine 2017;12:310-316. © 2017 Society of Hospital Medicine
© 2017 Society of Hospital Medicine
Statistical Analyses
We determined the proportion of patients with at least one PIP, as well as the proportion of all prescribing events that were potentially inappropriate. We used the Chi-square statistic and 2-sample t tests to compare the unadjusted associations between patient-level characteristics and receipt of at least 1 inappropriate prescription and prescribing event-level factors with inappropriate prescriptions. Given that first-year residents are more likely to be working overnight when most PIPs are prescribed, we performed a simple logistic regression of potentially inappropriate prescribing by level of training stratified by time of prescription. A multivariable random-intercept logistic regression model was used to assess the adjusted association between patient- and prescribing event-level characteristics with inappropriate prescribing, adjusting for clustering of prescribing events within patients. Characteristics of interest were identified a priori and those with significant bivariate associations with potentially inappropriate were selected for inclusion in the model. Additionally, we included time of prescription in our model to control for potential confounding. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc, Cary, North Carolina). The MSH Research Ethics Board approved the study.
RESULTS
Description of Patients Prescribed a Benzodiazepine Sedative Hypnotic
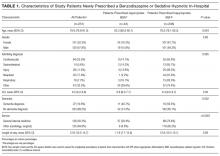
There were 1540 patients over the age of 65 discharged during the 4-month study period. We excluded the 232 patients who had been prescribed a BSH prior to admission. Of the remaining eligible 1308 BSH-naïve patients, 251 (19.2%) were prescribed a new BSH in hospital and were included in the study. Of this cohort of 251 patients, 193 (76.9%) patients were prescribed a single BSH during their admission while 58 (23.1%) received 2 or more. Of all eligible patients, 208 (15.9%) were prescribed at least 1 PIP. Approximately half of the cohort was admitted to the general internal medicine service, and the most common reason for admission was cardiovascular disease (Table 1).
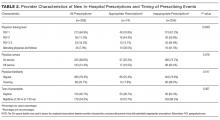
Description of Prescriptions of Benzodiazepine Sedative Hypnotic
We reviewed 328 prescriptions for BSH during the study period. The majority of these, 254 (77.4%) were potentially inappropriate (Table 2). The most common PIPs were zopiclone (167; 65.7%) and lorazepam (82; 32.3%). The PIPs were most frequently ordered on an as-needed basis (219; 86%), followed by one-time orders (30; 12%), and standing orders (5; 2%). The majority of PIPs (222; 87.4%) was prescribed for insomnia with a minority (32; 12.6%) prescribed for agitation and/or anxiety.
Most PIP were prescribed during overnight hours (159; 62.6%) and when an in-house pharmacist was unavailable (211; 83.1%). These variables were highly correlated with prescription of sleep aid, which was defined in our criteria as potentially inappropriate. Copies of discharge prescriptions were available for 189 patients. Of these 189 patients, 19 (10.1%) were sent home with a prescription for a new sedative.
Association Between Patient/Provider Variables and Prescriptions
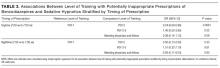
Patient factors associated with fewer PIPs in our bivariate analyses included older age and dementia (Table 1). A greater proportion of nighttime prescriptions were PIPs; however, this finding was not statistically significant (P = 0.067). The majority of all prescriptions was prescribed by residents in their first year of training (64.9%; Table 2), and there was a significant difference in rates of PIP across level of training (P = 0.0007). When stratified by time of prescription, there was no significant difference by level of training for nighttime prescriptions. Among daytime prescriptions, second-year residents and staff (attending physicians and fellows) were less likely to prescribe a PIP than first-year residents (odds ratio [OR], 0.24; 95% confidence interval [CI], 0.09-0.66 and OR, 0.39; 95% CI, 0.14-1.13, respectively; Table 3); however, the association between staff and first-years only approached statistical significance (P = 0.08). Interestingly, 20.4% of all PIPs were ordered routinely as part of an admission or postoperative order set.
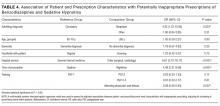
In our regression model, admission to a specialty or surgical service, compared to the general internal medicine service, was associated with a significantly higher likelihood of a PIP (OR, 6.61; 95% CI, 2.70-16.17; Table 4). Additionally, compared to cardiovascular admission diagnoses, neoplastic admitting diagnoses were associated with a higher likelihood of a PIP (OR, 4.43; 95% CI, 1.23-15.95). Time of prescription was a significant predictor in our multivariable regression model with nighttime prescriptions having increased odds of a PIP (OR, 4.48; 95% CI, 2.21-9.06,). When comparing prescribers at the extremes of training, attending physicians and fellows were much less likely to prescribe a PIP compared to first-year residents (OR, 0.23; 95% CI, 0.08-0.69; Table 4). However, there were no other significant differences across training levels after adjusting for patient and prescribing event characteristics.
DISCUSSION
We found that the majority of newly prescribed BSH in hospital was for the potentially inappropriate indications of insomnia and agitation/anxiety. Medications for insomnia were primarily initiated during overnight hours. Training level of prescribers and admitting service were found to be associated with appropriateness of prescriptions.