Anterolateral hip pain • no specific injury • Dx?
► Anterolateral hip pain
► No specific injury
THE CASE
A 22-year-old man presented to our family medicine clinic with hip pain of 2 weeks’ duration. The patient played hockey around the time of onset, but denied any specific injury. The pain, which affected the anterolateral aspect of the patient’s right hip, first started when he stood up after eating a meal. He rated the pain as an 8/10 on average and said that it was worse with movement. The patient had not shown improvement with conservative therapy (rest, ice, and ibuprofen). His medical and surgi
The physical exam revealed pain on active flexion and abduction of the hip. Passive range of motion (ROM) was negative for pain. The right hip was grossly normal with no pain on palpation or crepitus. There was no associated muscle tenderness. The patient was advised to continue to rest and ice the hip, as well as to take ibuprofen for pain relief. He was referred to Physical Therapy.
He returned to our clinic 4 weeks later with no improvement in his symptoms despite several sessions of physical therapy. We ordered radiographic images and magnetic resonance imaging (MRI) of the right hip.
THE DIAGNOSIS
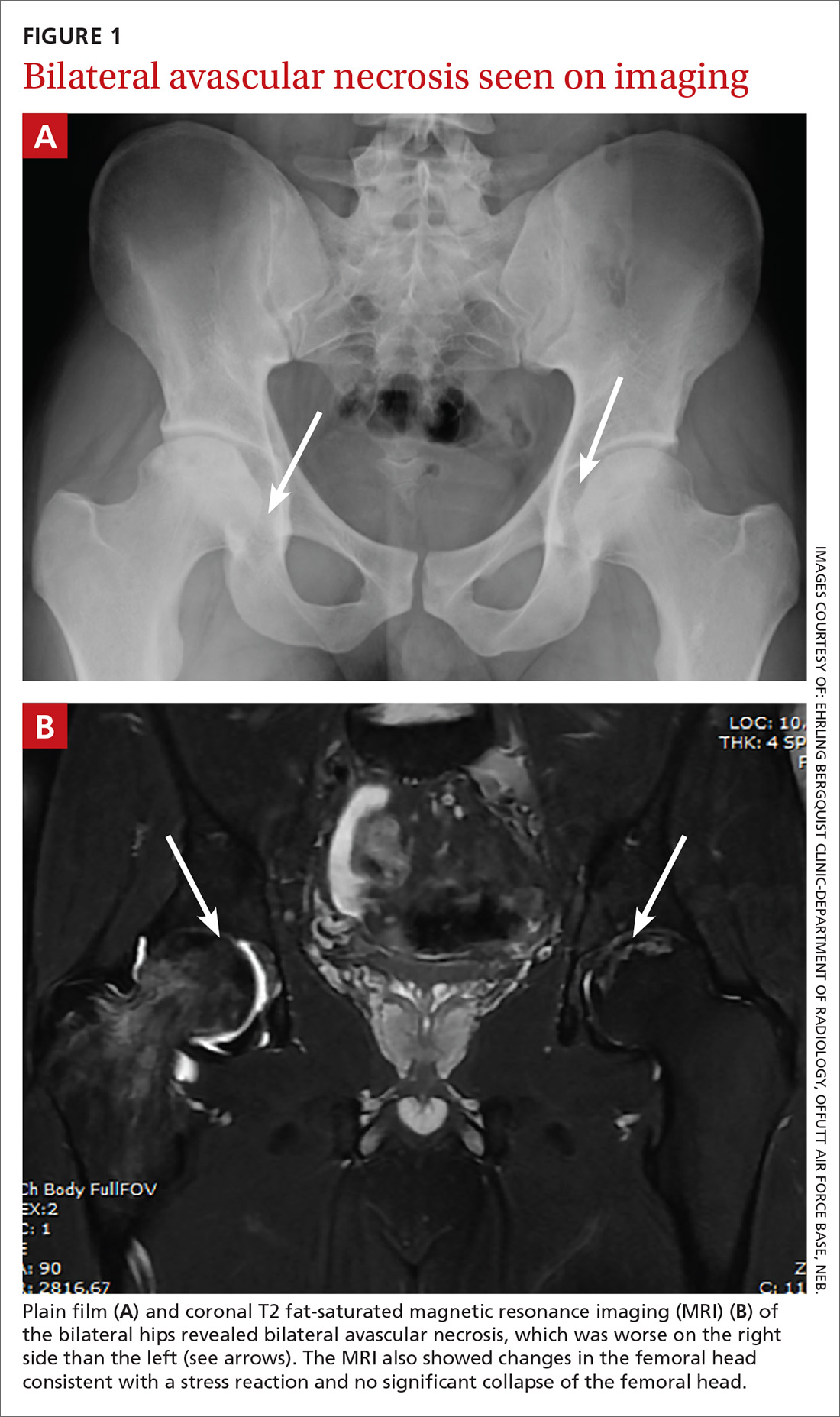
Plain films (FIGURE 1A) showed bilateral avascular necrosis (AVN) of the femoral heads, which was worse on the right side than the left. An MRI (FIGURE 1B) further supported this diagnosis, revealing changes in the femoral neck consistent with a stress reaction and no significant collapse of the femoral head.
DISCUSSION
AVN of the hip has an incidence ranging from 10,000 to 20,000 new cases annually.1,2 It has many possible causes, including trauma, systemic lupus erythematosus, glucocorticoid use, and chronic excessive alcohol use. Although the underlying pathophysiology varies, experts hypothesize that most cases are caused by a disruption of the blood supply, which leads to hyperemia and cortical destruction and collapse.1,2
Certain medications can cause AVN
A more thorough history-taking at this patient’s initial visit would have prompted imaging at that time and ensured that the standard of care was met. Upon further investigation at his follow-up appointment, it was discovered that he had been diagnosed with acute pre-B cell lymphoblastic leukemia (ALL) 2 years earlier and had undergone chemotherapy with cytarabine, vincristine, L-asparaginase, daunorubicin, methotrexate, and glucocorticoids. This discovery, along with the lack of symptom improvement, prompted the ordering of his imaging studies. Long-term glucocorticoid therapy is the second leading cause of AVN, following traumatic events.3 High daily dosages (>40 mg/d) and high cumulative dosages of glucocorticoids are associated with a significantly increased risk for AVN.4,5
The other chemotherapy agents with which our patient had been treated (cytarabine, vincristine, L-asparaginase, daunorubicin, and methotrexate) have no reported links to AVN. When mentioned in the literature, however, they are usually coupled with the use of dexamethasone or prednisone.
Continue to: One case report described a patient with...






