Comparing risk models guiding growth factor use in chemotherapy
Background The National Comprehensive Cancer Network (NCCN) and the American Society of Clinical Oncology (ASCO) have guidelines for using colony-stimulating factors (CSF) for chemotherapy-induced neutropenia (CIN). Both groups recommend CSF if the chemotherapy has a risk for febrile neutropenia of more than 20%. The guidelines are less definitive if the risk is intermediate (10%-20%). Two risk models developed by Hosmer and Bozcuk and their respective colleagues may provide guidance regarding CSF decision making in this intermediate risk population.
Objective To examine whether risk models developed by Hosmer and Bozcuk had adjunct value to the NCCN and ASCO guidelines when applied to patients with lung cancer who were receiving intermediate-risk chemotherapy.
Methods Male and female patients aged 18-75 years with a diagnosis of any stage lung cancer, small or non-small cell, who required and received their initial chemotherapy at Drexel University in Philadelphia were included in this study. Patients who received growth factor before their chemotherapy were excluded. The Hosmer and Bozcuk calculators for febrile neutropenia risk and the NCCN and ASCO guidelines for using CSF for CIN were applied to this group of patients.
Results 43 patients were included in the study. The Hosmer and Bozcuk calculators and NCCN and ASCO guidelines recommended giving CSF to 26, 22, 25, and 38 patients, respectively. The sensitivities for detecting severe CIN were 89%, 78%, 67%, and 97%, and the specificities were 44%, 56%, 45%, and 14%, respectively.
Limitations Small cohort size; data were limited in scope.
Conclusions In lung cancer patients receiving intermediate-risk chemotherapy, the Hosmer calculator had the best combination of sensitivity, specificity, and ease of use. The NCCN guidelines were less sensitive, whereas the ASCO guidelines were the least specific. Based on these findings, we recommend using the Hosmer calculator because it lends to accurate but judicious use of CSF.
Accepted for publication November 2, 2018
Correspondence Chetan Jeurkar, DO; jeurkar2@gmail.com
Disclosures The authors report no disclosures/conflicts of interest.
©2018 Frontline Medical Communications
doi https://doi.org/10.12788/jcso.0429
Methods
Study population
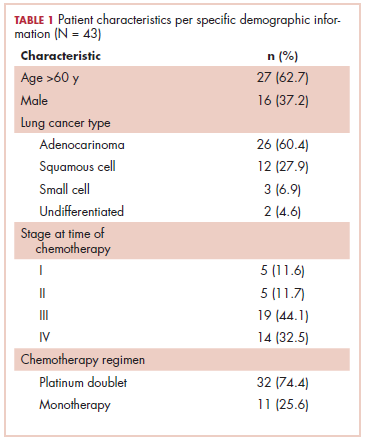
This was a cross-sectional, retrospective study looking at male and female patients aged 18 to 75 years who were treated in the hematology–oncology offices of Drexel University in Philadelphia, Pennsylvania, from 2005 through 2016, who had a diagnosis of lung cancer and were, at some point during their disease, treated with chemotherapy. By using ICD-10 codes for any type of lung cancer, we identified 242 patients. Of those, 106 patients were excluded because they had never received chemotherapy, 16 were excluded either because of miscoding of the type of cancer or because they never actually had cancer, and 61 were excluded either because chemotherapy had not been delivered at our institution or because there were insufficient data to apply the 2 risk models. Of the remaining 59 patients, 16 were excluded because they had received prophylactic CSF with their first cycle of chemotherapy, leaving a total of 43 patients to whom the various risk models and guidelines could be applied (Table 1). If any of the 43 patients were found to be neutropenic, they were given growth factor shortly thereafter.
Chemotherapy for these 43 patients consisted of either a platinum doublet (cisplatin or carboplatin with either etoposide, pemetrexed, gemcitabine, or paclitaxel) or monotherapy with either paclitaxel, abraxane, navelbine, or pemetrexed. Of the 43 patients, 32 had platinum-based doublets, and 11 had monotherapy with one of the listed agents (Table 1).
Formal patient consent was not required because this was a retrospective study.
Defining CIN and FN
Neutropenia was defined as an absolute neutrophil count (ANC) of less than 1500 neutrophils per microliter. The levels of neutropenia were defined as mild (ANC, 1000-1500 neutrophils/μL), moderate (ANC, 500-1000 neutrophils/μL), and severe (ANC, <500 neutrophils/μL). The NCCN guidelines define FN as a single temperature of >38.3°C orally or >38.0°C over 1 hour, with an associated ANC of <500 or <1000 with a predicted decline to <500 over the next 48 hours. 5
Risk models
It should be noted that the Hosmer and Bozcuk calculators were powered to detect occurrence of FN. 7,8 However, we also applied them for the risk of any CIN. In scoring for the Hosmer calculator, points are given to each risk factor and are added together to give a final risk score. This risk score correlates to a percentage of predicted FN. The score for the Hosmer calculator is from minus 18 to plus 19, in which a score of 13 or higher correlates to a 15% predicted risk of FN, and a score of 0 or less correlates to a 1.6% risk of FN. 7 For the Bozcuk calculator, a nomogram is used to calculate risk. Individual points are given to each risk factor and are then summed to give a total that correlates to a risk of FN. The score range for the Bozcuk calculator is 0 to 300, with a score of greater than 190 correlating to a greater than 90% risk of FN, and a score of 0 correlating to a 0% predicted risk of FN. 8