Patterns of malignancies in patients with HIV-AIDS: a single institution observational study
Background With the widespread use of antiretroviral therapy in patients with HIV-AIDS, a prolonged life expectancy is now evident. This has led to an increased incidence of malignancies in this patient population. The spectrum of malignancies in these patients differs worldwide.
Objective To study the patterns of AIDS-defining malignancies (ADMs) and non–AIDS-defining malignancies (NADMs) in patients in India with HIV-AIDS and to analyze the correlation of CD4 counts with the malignancies.
Methods This retrospective study included patients presenting with a malignancy and coexisting HIV-AIDS from January 2013 through December 2016. Patients with CD4 counts at the time of diagnosis of malignancy and having received treatment were analyzed. Analyses of the patient characteristics and correlation of CD4 counts with ADM and NADM were performed.
Results A total of 285 patients were evaluated. The median age was 44.8 years (range, 5-80 years). The mean CD4 count was 235.4 cells/mm3 (range, 50-734 cells/mm3; reference range, 500-1,500 cells/mm3). Cervical cancer was the most common malignancy in women, and non-Hodgkin lymphoma (NHL) was the most common among men. There was a statistically significant difference in CD4 counts between ADMs and NADMs (P = .03). A statistical difference was also noted when the CD4 counts of patients with NHL were compared with other malignancies. However, there was no statistically significant difference noted when CD4 counts of patients with cervical cancer were compared with NADM (P = .914).
Limitations This was a retrospective study and included only patients receiving treatment for malignancies at a single institution.
Conclusions NHL and cervical cancer continue to be the most common malignancies in patients with HIV-AIDS in developing countries. NHL tends to occur in patients with lower CD4 counts.
Funding/sponsorship None
Accepted for publication August 13, 2018
Correspondence
Deepak Koppaka, MD; Drdeepak.Koppaka@gmail.com
Disclosures The authors report no disclosures/conflicts of interest.
Citation JCSO 2018;16(4):e188-e192
©2018 Frontline Medical Communications
doi https://doi.org/10.12788/jcso.0416
Related content
Immunotherapy may hold the key to defeating virally associated cancers
Bilateral chylothorax in an AIDS patient with newly diagnosed Kaposi sarcoma
Metastatic Kaposi sarcoma with osseous involvement in a patient with AIDS
Submit a paper here
India has the third largest HIV epidemic in the world because of its large population size, with 0.3% of the adult population infected with HIV. That translates to 2.1 million infected people, posing a significant challenge in the management of these individuals.1 In all, 43% of the infected are currently on highly active antiretroviral therapy (HAART).1 There has been a significant decrease in the number of HIV-AIDS–related deaths in recent years because of the remarkable increase in the use of antiretroviral therapy.2 However, the prolonged life expectancy in these patients has resulted in an increase in the risk of various new diseases such as cancers. With the complex interactions between altered immunity and infections, the risk of cancers is markedly increased in patients with HIV-AIDS.3 The spectrum of malignancies in this group of patients differs from that in the general population. In addition, the pattern and the magnitude of malignancies differ in different parts of the world.4 In this study, we have analyzed the pattern of malignancies in patients with HIV-AIDS in a regional cancer center in India. The aim of the study was to analyze the pattern of malignancies in patients with HIV-AIDS based on their age and sex and to document the CD4 counts at the time the malignancy was diagnosed.
Methods
We retrieved data from our institution’s medical records department on all patients who had HIV-AIDS and had been diagnosed with a malignancy. Data of all patients presenting with a malignancy and coexisting HIV-AIDS from January 2013 through December 2016 were analyzed initially. Only patients for whom there was a documented CD4 count were included in the final retrospective analysis. We analyzed the correlation between the patients’ CD4 counts and malignancies subclassified as AIDS-defining malignancies (ADMs; aggressive B-cell non-Hodgkin lymphoma [NHL] and cervical cancer) or non–AIDS-defining malignancies (NADMs; all other malignancies other than aggressive NHL and carcinoma cervix were defined as NADM). We also analyzed the correlation between the CD4 count and NHL and other malignancies. A statistical analysis was performed using SPSS Statistics for Windows, version 23 (IBM Corp, Armonk, NY). The independent sample Mann-Whitney U or Kruskal-Wallis tests were used for comparing the CD4 counts between the various subgroups of malignancies. The study was carried out in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines.
Results
A total of 370 patients who were diagnosed with malignancy and have coexisting HIV-AIDS were identified. In all, 85 patients were excluded because there were no CD4 counts available for them, and the remaining 285 patients were included in the final analysis. Of that total, 136 patients (48%) were men, and 149 (52%) were women.
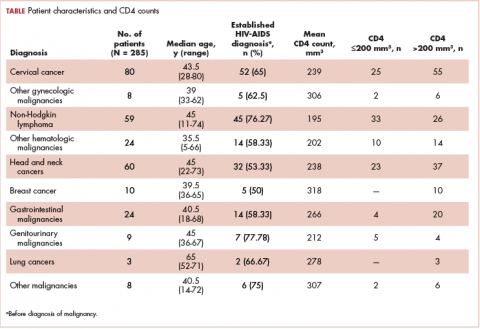
,The median age of the population was 44.8 years (5-80 years) at the time of diagnosis with malignancy. The mean CD4 count of the entire population was 235.4 cells/mm3 (50-734 cells/mm3). There were 104 patients with CD4 counts of ≤200 cells/mm3, and 181 patients had CD4 counts of >200 cells/mm3 (Table 1). All patients received the HAART regimen, efavirenz-lamuvidine-tenofovir (600 mg/300 mg/300 mg Telura).
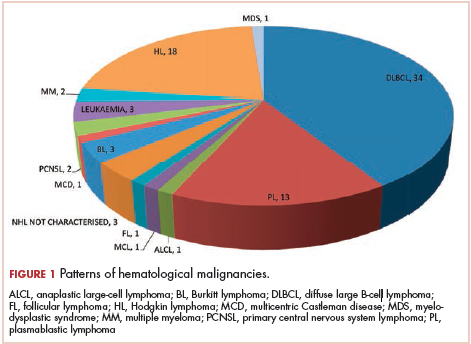
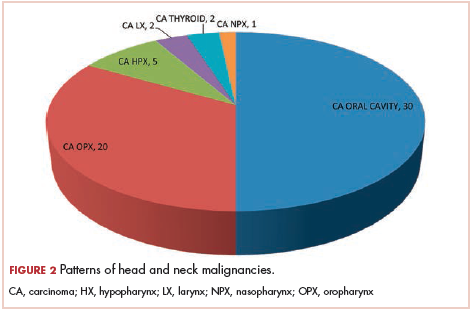
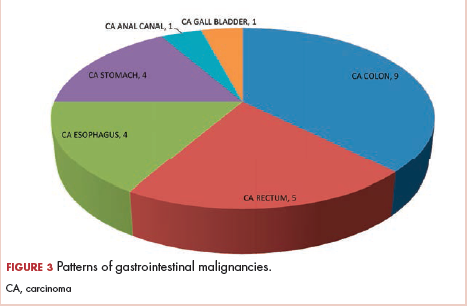
The most common malignancies in this population were gynecologic malignancies, followed by hematologic malignancies. Cervical cancer was the most common malignancy among women as well as in the overall study population. Among men, the most common malignancy was NHL. The second and third most common malignancies in men were carcinoma oral cavity and carcinoma oropharynx, respectively, whereas in women, they were NHL and breast cancer. The distribution of various hematologic, head and neck, and gastrointestinal malignancies in this group of patients is shown in Figures 1, 2, and 3.
The ADMs in the study were NHL, including 2 patients diagnosed with primary central nervous system (CNS) lymphomas, and cervical cancer. No case of Kaposi sarcoma, also considered an ADM, was identified in this study. The common NADMs include head and neck malignancies (Figure 2), gastrointestinal malignancies (Figure 3), gynecological and genitourinary malignancies, and breast cancer. The mean CD4 count in the ADM subgroup was 221 cells/mm3, and in the NADM subgroup, it was 250 cells/mm3. There was a significant difference in the distribution of CD4 counts between the ADM and NADM subgroups (P = .03; Mann-Whitney U test). A statistical difference was also noted when the CD4 counts of the patients with NHL were compared with other malignancies (P = .0001; Mann-Whitney U test) There was no statistically significant difference noted when CD4 counts of patients with cervical cancer were compared with NADMs (P = .914).