Analgesic management in radiation oncology for painful bone metastases
Background Radiotherapy (RT) effectively palliates bone metastases, but pain relief may be delayed and need analgesic management. National Comprehensive Cancer Network (NCCN) Guidelines for Adult Cancer Pain recommend alteration of analgesic regimen for a pain intensity rating (PIR) of ≥4/10 (range, 0-10; 0 denotes no pain and 10, worst pain imaginable).
Purpose To evaluate frequencies of analgesic regimen assessment and intervention in radiation oncology (RO) consultations for bone metastases and evaluate the impact of a dedicated palliative RO service.
Methods Investigators reviewed consultation notes for 271 patients with bone metastases who were treated at 2 cancer centers at time points before and after implementation of a palliative RO service at Center 1. The service had not been implemented at Center 2 during the study time periods. The analgesic regimen assessment rate was recorded for symptomatic patients, and the analgesic intervention rate was recorded for those with a PIR of ≥4.
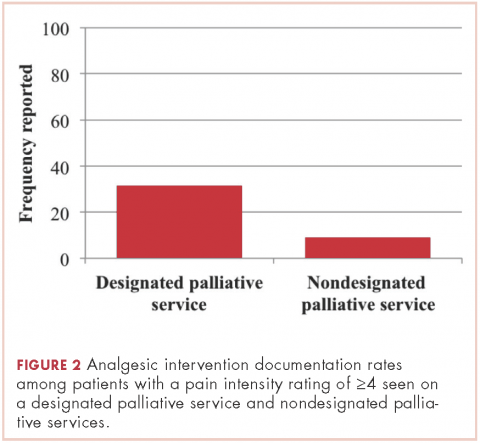
Results The median PIR for painful metastases was 5 (interquartile range [IQR], 2-7), and 51% of those assessed had a PIR of ≥4. Analgesic regimen was reported for 38% of symptomatic patients. Analgesic intervention occurred for 17% of patients with a PIR of ≥4. Palliative RO service patients had higher rates of analgesic assessment (59.5% vs 33.5%, respectively; P = .002) and intervention (31.6% vs 9.2%, P = .01) compared with those not seen in the service. There was no significant difference in analgesic assessment or intervention between nondedicated palliative RO care at the 2 centers.
Limitations Retrospective design, reliance on documentation for evaluating analgesic management
Conclusions At 2 cancer centers, half of the patients with bone metastases who received RT had a PIR of ≥4, yet only a minority had analgesic assessment and intervention, indicating a need for quality improvement in RO. Integrated palliative RO care is associated with improved analgesic management in accordance with NCCN guidelines.
Accepted for publication December 6, 2017
Correspondence michael.garcia@ucsf.edu
Disclosures The authors report no disclosures/conflicts of interest.
Citation JCSO 2018;16(1):e8-e13
©2018 Frontline Medical Communications
doi https://doi.org/10.12788/jcso.0388
Related article
Hospitalizations for fracture in patients with metastatic disease...
Submit a paper here
Methods
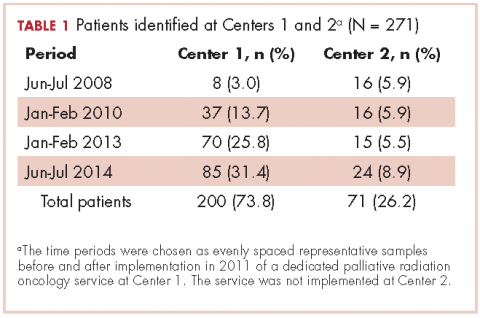
We searched our institutional databases for patients seen in RO consultation for bone metastases using ICD-9 code 198.5, and retrospectively reviewed consultation notes for those patients during June-July 2008, January-February 2010, January-February 2013, and June-July 2014. Those time periods were chosen as evenly spaced representative samples before and after implementation of a dedicated palliative RO service in 2011 at Center 1. Center 2 did not implement a dedicated palliative RO service in these time periods.
Within consultation notes, we recorded the following data from the History of the Present Illness section: symptoms from bone metastases (symptomatic was defined as any pain present); PIR (range, 0-10); and whether or not the preconsultation analgesic regimen was reported for symptomatic patients (including analgesic type, dosing, effectiveness, and adherence).
Documentation of the analgesic regimen in the history section of the notes was considered the proxy for analgesic regimen assessment at time of RO consultation. Analgesics within the Medications list, which were autopopulated in the consultation note by the electronic medical record, were recorded.
,Whether or not pain was addressed with initiation or titration of analgesics for patients with a PIR of ≥4 was recorded from the Assessment and Plan portion of the notes, and that metric was considered the proxy for pain intervention. In addition, the case was coded as having had pain intervention if there was documentation of the patient declining recommended analgesic intervention, or the patient had been referred to a symptom management service for intervention (eg, referral to a specialty palliative care clinic), or there was recommendation for the patient to discuss uncontrolled pain with the original prescriber. A PIR of 4 was chosen as the threshold for analgesic intervention because at that level, NCCN guidelines for cancer pain state that the analgesic regimen should be titrated, whereas for a PIR of 3 or less, the guidelines recommend only consideration of titrating the analgesic. Only patients with a documented PIR were included in the pain intervention analysis.
Frequencies of analgesic assessment and analgesic intervention were compared using t tests (Wizard Pro, v1.8.5; Evan Miller, Chicago IL).
Results
A total of 271 patients with RO consultation notes were identified at the 2 centers within the 4 time periods (Table 1).
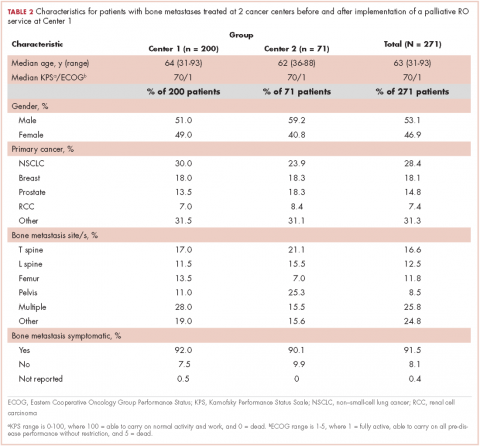
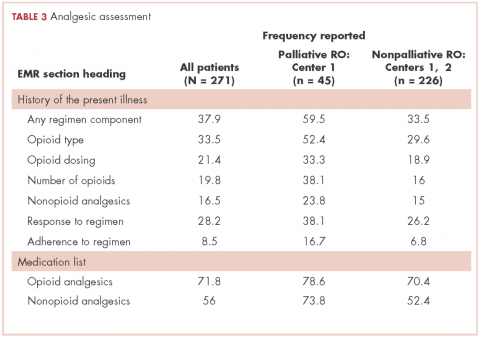
Among symptomatic patients, any component of the preconsultation analgesic regimen (including analgesic type, dosing, pain response, and adherence) was documented for 37.9% of the entire cohort at RO consultation (Table 3). At Centers 1 and 2, the frequencies of analgesic regimen assessment were documented for 41.3% and 28.1%, respectively (P = .06). Among symptomatic patients, 81.5% had an opioid or nonopioid analgesic listed in the Medications section in the electronic medical record at time of consultation.
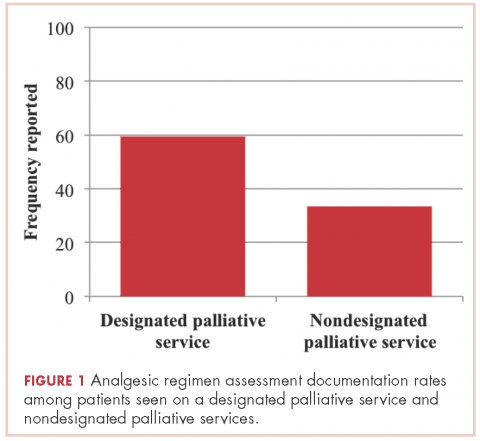
Patients seen on the dedicated palliative RO service at Center 1 had an analgesic assessment documentation rate of 59.5%, whereas the patients not seen on a palliative RO service (ie, patients seen on a nonpalliative RO service at Center 1 plus all patients at Center 2) had an assessment documentation rate of 33.5% (P = .002; Figure 1). There was no significant difference between rates of analgesic regimen assessment between patients seen at Center 2 and patients seen within nondedicated palliative RO services at Center 1 (28.1% vs 35.9%, respectively; P = .27).
In patients seen at Center 1 only, those seen on the palliative RO service had a higher documentation rate of analgesic assessment compared with those seen by other services after implementation of the dedicated service (59.5% vs 38%, respectively; P = .018). Time period (after versus before 2011) was not significantly associated with the rate of documentation of analgesic assessment at either Center 1 (after vs before 2011: 44.4% vs 31%, P = .23) or Center 2 (31.4% vs 24.1%, P = .60).
Among patients with a PIR of ≥4, analgesic intervention was reported for 17.2% of patients within the entire cohort (20.8% at Center 1 and 0% at Center 2, P = .05). Among those with a PIR of ≥4, documentation of analgesic assessment noted in the History of the Present Illness section was associated with increased documentation of an analgesic intervention in the Assessment and Plan section (25% vs 7.3%; odds ratio [OR], 4.22; 95% confidence interval [CI], 1.1-16.0; P = .03).
Patients seen on the dedicated palliative RO service at Center 1 had a documented analgesic intervention rate of 31.6%, whereas the patients not seen on a palliative RO service (ie, those seen on a nonpalliative RO service at Center 1 plus all patients at Center 2) had a documented analgesic intervention rate of 9.2% (P = .01; Figure 2). There was no statistically significant difference between rates of documentation of an analgesic regimen intervention between patients seen at Center 2 and patients seen within nondedicated palliative RO services at Center 1 (0% vs 17.2%, respectively; P = .07).
Looking at only patients seen at Center 1, patients with a PIR of ≥4 seen on the dedicated palliative RO service had a nearly significant higher rate of documented analgesic interventions in the time period after implementation of the dedicate service (31.6% if seen on the dedicated service vs 12% if seen on a nondedicated service, P = .06).