From angst to analytics: lessons learned from an oncology care model internal pilot
Thirteen practices affiliated with the US Oncology Network (USON) were invited to participate in the Oncology Care Model (OCM), a value-based care initiative that required changes in the following domains: 24/7 coverage, electronic health records (EHR) certification, navigation and care coordination, continuous quality improvement, incorporation of the Institute of Medicine Care Plan, and adherence to nationally recognized guidelines. Although 24/7 physician coverage, access to EHR, and adherence to guidelines were routine for these practices, the other requirements represented significant challenges. To be prepared for this transformative opportunity, USON implemented a pilot program 4 sites 6 months before participation began to identify the practice changes that would be needed to meet OCM requirements with the goal of standardizing best practices that would be shared with other USON sites. Through the pilot, the practices developed team-based approaches for navigation, the treatment plan, team-based care, and a core technology platform to address extensive OCM documentation requirements. An ongoing challenge is addressing the cultural resistance to change, which can hopefully be addressed with data and outcomes. Unexpected findings included the difficulty in identifying eligible candidates, a need to increase emphasis on adherence to national guidelines, and a need for strategies to reduce hospitalizations and emergency department visits. The pilot program showed that several seemingly challenging aspects of the OCM were feasible and areas for improvement were identified for improving the patient experience while decreasing the cost of cancer care.
Accepted for publication September 14, 2017
Correspondence Marcus A Neubauer, MD; Marcus.Neubauer@Mckesson
Disclosures The authors report no disclosures/conflicts of interest.
Citation JCSO 2017;15(6):e297-e302
©2017 Frontline Medical Communications
doi https://doi.org/10.12788/jcso.0371
Submit a paper here
The OCM and practice readiness
As a part of the CMS proposal process, practices were required to submit implementation plans by June 30, 2015. The purpose of the implementation plan was to define how a practice could transform over 6 broad domains: 24/7 coverage; EHR certification; navigation and care coordination; continuous quality improvement; incorporation of the Institute of Medicine’s (IOM’s) Care Management Plan; and adherence to nationally recognized guidelines. The periods of patient eligibility for the program were 6-month treatment episodes triggered by a cancer diagnosis, a provider encounter claim, and a Part B or D drug claim specifically identified as a cancer treatment. The episodes could be repeated if the 3 criteria continued to be met. All charges continued to be billed as fee-for-service as before, but in addition, participating practices could bill a monthly enhanced oncology services (MEOS) payment for the duration of an episode. Reducing the total cost of care while meeting performance metrics thresholds would also qualify a practice for performance-based payments.
Of the primary components, EHR certification and adherence to guidelines had been addressed previously, but the other domains represented significant challenges. Although 24/7 physician coverage with access to an EHR is standard for all practices, most practice sites do not have an insight into the frequency of hospital admissions, the ability to efficiently add sick patients to the daily schedule, or a routine call system to assess chemotherapy toxicity.
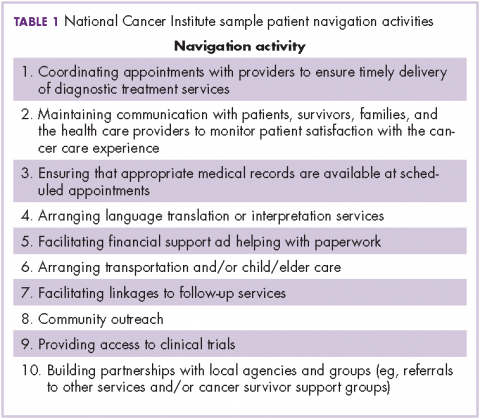
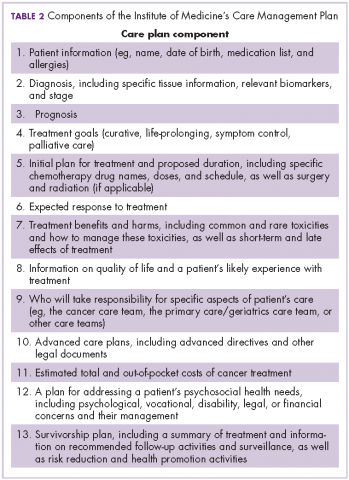
The OCM proposes 10 potential navigation/care coordination functions (Table 1) and does not consider those functions to be the role of one person, but rather a team responsibility. Most of our practices perform at least some of these functions, but they are not formally designated, coordinated, or recorded. A similar condition exists for the IOM care plan, which includes recommendations for treatment and adverse event management (Table 2). The prognosis, toxicity, quality-of-life, and goals-of-care requirements are often found in the physician notes, but not systematically documented or searchable.
Similar challenges have been observed for continuous quality improvement programs. Although the data are available, they are often not easy to search and, therefore, are difficult to retrieve and report. The OCM, as with any transformational program, must always weigh the benefit of information with the burden of consumption of physician and staff time to collect and input these data.18
Prepilot project work
In October 2015, lead physicians and managers from the 12 participating practices were brought together with analytic, technical, process management, and business experts from USON and McKesson Specialty Health. The objective of the meeting was to define the areas of greatest need for day 1 of the OCM and to be prepared. The challenges were to identify the changes needed to meet the requirements of the OCM while improving the patient experience, sustaining the viability of the community oncology practices, creating teams to deliver more effective care, and using data to bend the cost curve. Accordingly, 4 work streams were created: Care and Support; Content; Technology; and Communications, Revenue Cycle and Incentives.
Care and Support
The key tasks of the Care and Support team were to define the workflows for navigation and the IOM care plan. As a patient’s journey through the clinic was mapped out, it became clear that although multiple personnel could participate in the navigation and care plans, there was no systematic way to organize and record the components of successful navigation. The goals for the pilot were to test various options for navigation and to identify best practices that could be translated into standard operating procedures.
Content
The Content team was charged with identifying available programs that would fit into the OCM requirements. These included advance care planning, survivorship, chemotherapy teaching, risk assessment, pathways, and symptom assessment. A longer-term goal was the development of care paths, a more comprehensive map of the patient’s journey that would include consultations, coordinated care, imaging, labs, and other services.
Technology
The task for the Technology work stream was to identify processes of care that required documentation and to evaluate current and future technology solutions to improve efficiencies. The electronic medical record satisfied for the input of data with relevant clinical details, demographics, disease types, and staging. A web-based pathways tool supported clinical decision-making, as well as compliance to pathways. The Medicare quality metric programs set the stage for development of capture and reporting tools for data from many sources. The pilot would indicate the adequacy of these tools and the need for expansion or development of new functions or programs. Of particular importance was recording the IOM care plan and navigation functions in a searchable format. As care paths are developed, risk prediction, palliative care, and other services need to be encompassed. Finally, technology will support the identification and enrollment of eligible patients, and billing activities.