Goals-of-care discussions
Goals-of-care conversations led by the oncologist are key to advancing the prognostic awareness of the patient and family, but too frequently do not occur or are ineffective in leading to advance care planning and appropriate planning for end-of-life care. At our institution, a phase 3 trial of palliative care added to usual care of phase 1 clinical trial patients gave us the opportunity to
develop an electronic medical record–based goals-of-care template for discussions. We can complete all or parts of the form with patients, use it to ensure full coverage of important tasks such as planning for transition to hospice and legacy work, and make sure all the providers are 'on the same page' about treatment plans. We have this within our EMR as a SmartPhrase that can be brought up for completion, and have found that it helps to clarify patient understanding. The form can also be used to document advance care planning for both clinical care and billing. Although this tool has not been formally tested, we have found that it is effective in day-to-day practice as well as in research, and we share it here.
Accepted for publication May 15, 2017
Correspondence Thomas J Smith, MD; tsmit136@jhmi.edu
Disclosures The authors report no disclosures/conflicts of interest.
Citation JCSO 2017;15(4):e190-e194
©2017 Frontline Medical Communications
doi: https://doi.org/10.12788/jcso.0355
Related articles
Survivorship care planning in a comprehensive cancer center using an implementation framework
Initiating palliative care conversations: lessons from Jewish bioethics
Submit a paper here
Goals-of-care conversations led by the oncologist are a key opportunity to improve advance care planning and end-of-life care,1 but our patients are not understanding the essentials. Findings from a study of patients’ expectations about chemotherapy showed that more than two-thirds of patients with lung or colorectal cancers thought their palliative chemotherapy,2 radiation, 3 and/or surgery4 could cure them. Failure to effectively educate patients can lead to end-of-life care associated with poor quality of care, including over-aggressive care, poor quality of life with suboptimal symptom management, caregiver distress, and other potentially preventable problems.5
Palliative care routinely includes goals-of-care (GoC) discussions as part of the standard note. At one large urban hospital, the 30-day readmission rate was 10% if palliative care consultation was done, compared with 15% if no consultation was obtained.6 Patients who had consultations that included GoC discussions in addition to a symptom management consultation had a lower hospital readmission rate of 5%, compared with 15% in patients who received symptom management consultations alone (adjusted odds ratio [AOR], 0.36; confidence interval [CI], 0.27-0.48; P < .001). 6 Findings from another study showed that the use of aggressive end-of-life care was reduced by one-third when the patient and provider had a GoC planning session close to the time of diagnosis, instead of at the end of life.7
We prepared a template to be incorporated into the electronic medical record (EMR) to facilitate GoC discussions between the oncologist and patient as part of a randomized phase 3 trial of early versus delayed palliative care for phase 1 clinical trial patients. Documentation is one of the most important elements of efforts to improve end-of-life care, along with advance care planning, GoC discussions, and understanding the system of care.8 Because we have found this approach useful in our everyday oncology practice, we are sharing this simple, doable template in the hope that others will find it effective.
,The GoC template
What does it look like?
We developed a document for oncology GoC discussions that was incorporated into the EMR (Table). We use the GoC document in much the same way we’d review a computed-tomography scan with our patients and their families: we bring it up on the computer screen, show them the categories, and type in responses on the allotted spaces on the right-hand side of the document. The input can be done in real time or after the conversation, or even after the patient has left. In our practice, we access the Patient Instructions part of the EMR, use a SmartPhrase to copy the Word template into the chart, and start typing.
The completed GoC sheet can be used in several ways. Most commonly, we print it out for the patient and family, so that everyone has access to the same information. Printing it out as part of the after-visit patient summary also satisfies the meaningful use requirement for EMRs. It is also possible to cut and paste the document into a letter to the care team, or directly into the Progress Note, so that it will be available for members of the care team to see.
The GoC form does take some time to complete. Palliative care teams that have reported on what was done during the palliative care visit have noted that the initial and subsequent visits took about an hour, with about 20 minutes devoted to symptom management, 15 minutes to patient and family coping, and 10 minutes to illness understanding and education, including prognosis.9,10 In our own practice, we do questions 1-9 first (Table, shaded area) because it takes less time than anticipated, just like code status discussions,11 and it is much easier with a script.
We use this template for in- and out-patient consultations and for routine visits when a GoC discussion is warranted. It is important to remember that doing this counts as advance care planning and can be billed using the ACP codes.
How do you use template?
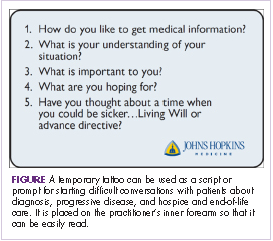
It is critically important to make sure that the patient and family are ready for this discussion. To further facilitate the discussion, we have devised a temporary palliative care tattoo with a script, or prompts, for what questions to ask and in what order they should be asked (Figure). The easy-to-read tattoo is worn on the inner forearm so that it is readily visible to the oncologist or advanced practice nurse.12
We always start by asking, “How do you like to get medical information?” (Table, question 1) and follow up with something like, “Are you the sort of person who wants all the details, or not?” (Table). If the response is yes, they want all the details, then we follow up with another question, “Does that include talking about prognosis and what might happen?” (Table). Most patients will want full disclosure of their circumstances and prognosis, but some will not, and will feel overwhelmed and disempowered if you proceed.
After reviewing the answers to question 1 and any follow-up questions you may have asked, you will be able to gauge whether you should continue with questions 2-4 in the template. Once you know more about the patient and the family’s understanding of the situation (Table, question 2), what is important to them (question 3), what they are hoping for (question 4), and have spoken to them about disease progression, recapped their treatment to date, and checked to see if they might be eligible for any clinical trials (question 5), it will be easier to move on to the next questions, about progressive disease and advance care planning: “You are doing OK now, but have you thought about a time when you could be sicker [and need] a living will or advance directive [question 6, see next section of this article]?” For people unwilling to have this discussion, or have it at that moment, there is an excellent article that outlines the process to help practitioners increase prognostic awareness.14 Patient readiness will change over time as they adjust to the life changes forced by serious illness, and one can put off the discussion until they are more accepting. Just remember that patients are not likely to broach the subject themselves, and part of our job is to offer guidance.
As Singh and colleagues have noted, many patients with incurable disease have poor “prognosis awareness,” 15 so it is important for the oncologist to have a GoC conversation with the patient to be able to guage the patient’s understanding of the prognosis after a scan that shows progressive disease. Singh and his colleagues reported that of 64 taped oncologist-patient conversations about scan results, only 4 included frank discussions about prognosis. The authors suggested asking the question, “Would you like to talk about what this means?” after showing the patient the scan to allow the patient some control and to get permission to disclose crucial information based on the reading of the scan.15
Getting started on the GoC discussions may be the hardest part. Some useful introductory lines might include: “In my experience, it is easier to talk about our goals of care while people are still doing well. I know the future can be more uncertain. That’s why I want us to discuss these things now,” or “I am worried about you, after looking at these scans. I think it is time to have another discussion about what the future holds.”