Defecation Disorders: Diagnosis and Treatment
From the Digestive Health Center, Medical College of Georgia, Georgia Regents University, Augusta, GA
Defecation is a coordinated process that involves generation of sufficient propulsive forces in the abdomen and rectum together with relaxation of the puborectalis and external anal sphincter. Likewise, continence involves conscious retention of bowel contents until stool or gas can be voluntarily eliminated in an appropriate fashion. A failure of these processes leads to altered bowel function and disorders of defecation that are commonly encountered in clinical practice. They include a diverse group of maladies that result in altered defecation. Among them are functional disorders, such as dyssynergic defecation, and mechanical/structural disorders, such as rectocele, solitary rectal ulcer syndrome (SRUS), excessive perineal descent, and rectal prolapse. This article discusses 3 cases that illustrate the clinical features and management approaches to dyssynergic defecation, SRUS, and fecal incontinence.
Case Study 1
Presentation and History
A 26-year-old white woman with a 10-year history of constipation presents to a gastroenterologist after referral from her primary care physician. She reports spontaneous bowel movements once every 2 weeks, and often she has to induce stools by using enemas or suppositories. Stooling became progressively more difficult for her during her teenage years, with infrequent bowel movements and hard stools (type 1–2 on Bristol stool scale). She also reports having to strain excessively during bowel movements, and on average she spends 30 minutes in the bathroom. She denies experiencing any perianal pain or bleeding or using manual maneuvers to defecate, but she often feels a sense of incomplete evacuation. She also describes intermittent abdominal pain and bloating.
She has tried several over-the-counter laxatives, includ-ing milk of magnesia, senna, and magnesium citrate. Most recently, she tried lubiprostone and polyethylene glycol without improvement. Her past medical history is significant for endometriosis, exploratory laparotomy, and 1 vaginal delivery. There is no family history of colorectal cancer or inflammatory bowel disease. She works as a truck driver and does not use alcohol, illicit drugs, or tobacco. There is no history of physical or sexual abuse. Her current medications include lubiprostone 24 µg twice daily, polyethylene glycol 17 g twice daily, and a birth control pill.
Physical Examination
On physical examination, the patient appears healthy without any distress. Her body mass index is 26 kg/m2, and vital signs are normal. General examination is normal. Abdomen is flat, and bowel sounds are normal. Mild tenderness is noted in both lower quadrants. Rectal examination reveals normal anal skin folds. Digital exam-ination reveals a normal resting tone with pellet-like stool that is heme-negative. When asked to attempt defecation, she shows poor perineal descent and paradoxical contraction of the anal sphincter.
Laboratory Evaluation
Laboratory testing reveals normal levels of thyrotropin and thyroxine, no anemia on complete blood count, and normal levels of calcium, glucose, and electrolytes.
What are the possible causes for this patient’s altered bowel habits?
What is the approach to physical examination in patients with constipation?
Causes of Constipation
Constipation is a common digestive disorder, affecting up to 20% of the world’s population [1]. Primary or idiopathic constipation consists of 3 common overlapping subtypes: slow-transit constipation, dyssynergic defecation, and constipation-predominant irritable bowel syndrome. Slow-transit constipation involves the slow movement of stool through the colon. This is usually seen on a colonic transit study or with wireless motility capsule study. Dyssynergia in general is caused by functional outlet obstruction with or without normal colonic transit. Patients with dyssynergia often complain of incomplete evacuation, excessive straining, bloating, and blockage [2]. Often patients with dyssynergia resort to manual disimpaction/vaginal splinting and/or abdominal pressure to facilitate bowel movements. Secondary constipation may result from metabolic disorders (eg, hypercalcemia and hypokalemia, disorders associated with renal failure, hypothyroidism, and diabetes) as well as medications, including narcotics, anticholinergics, and antidepressants.
Rectal Examination
Physical examination in patients with constipation should include a detailed rectal examination. The perianal skin should be inspected closely for fissures, fistulae, and skin excoriation. The anocutaneous reflex should be checked along with resting and squeeze anal tone. A study by Rao et al[3] showed that rectal examination could identify 76% of patients with dyssynergia. The sensitivity and positive predictive value for diagnosing dyssynergia with digital rectal examination was 81% and 99%, respectively, making it a good screening test for dyssynergia [3].
When is colonoscopy indicated in the workup of constipation?
What imaging studies may be useful?
Colonoscopy
Colonoscopic evaluation is only indicated in patients with alarming features such as rectal bleeding, weight loss, unex-plained abdominal pain, palpable mass in the abdomen or rectum, persistent and unexplained anal/rectal pain, or anemia, as well as in patients over age 50 years [4].
Colonic Transit Study
Two imaging studies can be useful in the evaluation of a patient with constipation: colonic transit study and defeco-graphy. A colonic transit study provides useful information regarding the rate at which stool travels through the colon. This test is performed by administering one capsule (Sitzmarks, Konsyl Pharmaceuticals, Fort Worth, TX) containing radiopaque markers. A plain radiograph of the abdomen is obtained on day 6 (120 hr after ingestion of capsule). A transit study is considered abnormal if more than 20% of markers (> 5) are present on a plain radiograph of the abdomen. Approximately two-thirds of patients with dyssynergia have an abnormal colonic transit study, with retention of markers either in the rectosigmoid region or throughout the colon [5]. Wireless motility capsule is a newer test that is comprised of ingesting a capsule and wearing a recorder for up to 5 days. This test measures regional transit (ie, gastric emptying, colonic transit time, and whole gut transit time), is standardized and validated, and avoids use of radiation [6].
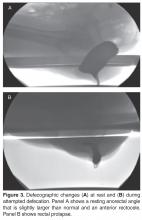
Defecography
Defecography is conducted by instilling a barium paste in the rectum and monitoring evacuation of the barium radiologically. It can reveal poor activation of the levator ani muscles, prolonged retention of the barium, inability to expel the barium, absence of a striping wave, rectal mucosal intussusception, rectocele, abnormal perineal descent, or rectal prolapse [5]. Although abnormalities are frequently found on defecography, they may not translate into clinical dysfunction. In one study, 77% of women with complaints of defecation disorders had abnormalities on defecography, but there was no relationship between the abnormalities and the patients’ symptoms [7]. Hence, defecography is not recommended unless there is clinical suspicion of prolapse or excessive descent. Endoanal and dynamic pelvic magnetic resonance imaging (MRI) can evaluate global pelvic floor anatomy in dynamic function [8]. Dynamic MRI in the seated position provides the most physiologic approach.
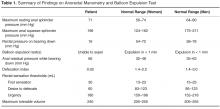
What testing is needed to make a diagnosis of dyssynergic defecation?
Both an abnormal balloon expulsion test and an abnormal pattern of defecation on anal rectal manometry are required to diagnose dyssynergic defecation [9]. Anorectal manometry provides information regarding rectal and anal pressures at rest and during maneuvers of simulated defecation as well as information on rectal sensation, rectoanal reflexes, and compliance [2,10]. There are 4 patterns of dyssynergia found on anorectal manometry: type 1, normal push effort with paradoxical contraction of the anal sphincter; type 2, poor push effort with paradoxical contraction of the anal sphincter; type 3, normal push effort with incomplete or absent relaxation of the anal sphincter; and type 4, poor push with incomplete anal relaxation. The balloon expulsion test should be included in the work-up of dyssynergia.
Normal subjects can expel a 50-mL water-filled balloon in less than 1 minute. Although normal patients can show a dyssynergic pattern in the left lateral decubitus position, when seated on a commode and with a sensation of stooling most exhibit a normal pattern of defecation [9].
Diagnosis
What treatment options are available for dyssynergia?
The treatment of patients with dyssynergic defecation consists of standard therapies for constipation, including diet, laxatives, and timed toileting. Medical therapy includes laxatives, polyethylene glycol, and lubiprostone.
Case Study 2
Initial Presentation and History
A 39-year-old woman presents with a 5-year history of intermittent bright red blood with stooling. Most often, she notices blood on the toilet paper or when wiping and rarely in the commode. She reports having experienced difficulty with bowel movements since her teens. She does not have a daily urge but strains up to 30 minutes to pass stool that is hard in consistency (type 1–2 on the Bristol stool scale). Over the past year, she has started using fingers to remove stool.
The patient reports bloating and abdominal discomfort that is improved with stooling. Her weight has been stable. Current medications include polyethylene glycol 17 g twice daily, sodium docusate 100 mg twice daily, iron sulfate 325 mg 3 times daily, and a birth control pill. Her past medical history is significant for iron deficiency anemia. Family history is notable for her mother and sister with similar “bowel troubles,” but no family history of inflammatory bowel disease or colorectal cancer. She is a salesperson and has been married for 7 years. She does not use tobacco or alcohol. As a child, she was sexually abused. She did not receive any formal counseling for the abuse. Review of systems is negative.
Physical Examination
General and neurologic examinations are normal. The abdomen is mildly distended, bowel sounds are normal, there is mild tenderness, and stool is palpable in the left lower quadrant. Rectal examination reveals normal anal skin with no fissures, intact anocutaneous reflex, and hard stool in the rectal vault that is guaiac-positive. The resting anal sphincter tone is elevated, and when asked to attempt defecation, there is excessive perineal descent and rectal mucosal intussusception with paradoxical anal contraction.
Laboratory Evaluation and Endoscopy
What is SRUS and how is it diagnosed?
Evaluation and Diagnosis
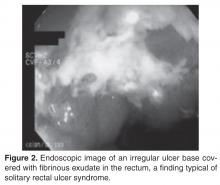
SRUS is characterized by single or multiple ulcerations of the rectal mucosa along with distinct pathologic changes [17]. The term solitary rectal ulcer is a misnomer because many patients have more than 1 lesion, and it is not always an ulcer. Patients with SRUS present with several symptoms, but the most common is passage of blood or mucus, and up to 26% may be asymptomatic [18]. The pathophysiology of this condition is poorly understood. Multiple mechanisms have been implicated, including occult or overt rectal prolapse, dyssynergia, rectal mucosal intussusception, rectal hypersensitivity with a persistent feeling of a need to defecate, and reduced mucosal blood flow [19].
The diagnosis of SRUS is based on the patient’s clinical history combined with endoscopy and histopathology findings. Endoscopically, the lesions may vary in appearance. Shallow ulcerations on hyperemic surrounding mucosa located on the anterior wall is the most common finding [17]. Lesions vary in size, although most are 1 to 1.5 cm in diameter [17] and rarely involve more than half the circumference of the rectal wall. Polypoid lesions occur in approximately 25% of patients with SRUS, and multiple lesions occur in 30% [17].
Obtaining specimens for histology is an important step in the evaluation of SRUS. The differential diagnosis includes Crohn’s disease, ulcerative colitis, ischemic colitis, and malignancy. The typical histologic findings include fibromuscular hyperplasia with smooth muscle infiltration of the lamina propria, thickening of the muscularis mucosa, regenerative changes, and distortion of the crypt architecture [17].
Are physiologic or imaging studies helpful in the diagnosis of SRUS?
Two complementary physiologic tests for SRUS are anorectal manometry and defecography. Anorectal manometry often shows evidence of dyssynergia and rectal hypersensitivity in patients with SRUS [20,21]. Hyper-sensitivity may produce a sensation of incomplete evacuation, which in turn results in excessive straining. Defecography may reveal rectal mucosal intussusception or overt rectal prolapse. The patient in this case had evidence of rectal hypersensitivity on anorectal manometry along with excessive perineal descent on defecography.
What are treatment options for SRUS?
Treatment of SRUS is not standardized. The options include topical medical therapy, biofeedback, and surgery. Uncontrolled studies have suggested that 5-aminosalicylic acid enema [22], sucralfate enema [23], steroid enema [24], and fibrin glue [25] may improve symptoms. Patients who fail topical therapy and have evidence of dyssynergia on anorectal manometry should receive biofeedback therapy. A case-control study of biofeedback involving 11 patients with refractory SRUS and 15 healthy controls showed improvement in anorectal function, including dyssynergia [21]. At follow-up endoscopy, 36% had complete mucosal healing and more than 50% showed partial healing. In a study involving 16 patients with SRUS and 26 healthy controls, Jarrett et al [26] showed that 75% of patients who underwent biofeedback therapy had improved and 31% had ulcer resolution. Surgical therapy should be considered in rare patients who are refractory to medical therapy. The Delorme procedure is commonly performed with a success rate of 42% to 100% [27].
The case patient underwent biofeedback therapy, and after 5 sessions had complete healing of the lesion and resolution of rectal bleeding and bowel symptoms.
Case Study 3
Initial Presentation and History
A 75-year-old woman is referred to a gastroenterologist with complaints of incomplete stool evacuation and intermittent fecal seepage. She passes stools daily but sits on the toilet for 15 to 20 minutes, and after straining will pass only a small amount of stool. She describes stools as type 4 on the Bristol scale with no blood or mucus. One to 2 hours after a bowel movement, she experiences some wetness in the perineal region and upon checking often notices that a tablespoon full of stool material has leaked out. Sometimes, she will pass another large stool. She denies any leakage of stool while sleeping. Occasionally, she has urgency and leaks stool before reaching the toilet. In the past, she has used digital maneuvers to facilitate stooling. This problem has interfered with shopping, socializing, and taking vacations.
Her past medical history is significant for narcolepsy, hypertension, tubal ligation, appendectomy, and inguinal hernia repair. Obstetric history is significant for 6 vaginal deliveries, 1 requiring episiotomy but no forceps use. Her current medications include estradiol vaginal cream, hydrochlorothiazide, pilocarpine, and amitriptyline 10 mg 3 times daily. She also reports stress urinary incontinence, particularly with sneezing and coughing.
Physical Examination
Physical examination reveals a well-nourished woman with normal vital signs and a normal general examination. Abdominal examination is normal. A rectal examination shows no fissures, but the anocutaneous reflex is absent on the right side. Resting and squeeze sphincter tones are normal, with good perineal descent and normal anal relaxation.
Laboratory Evaluation
What are the mechanisms involved in fecal incontinence?
What are the 3 clinical subtypes of fecal incontinence?
Mechanisms and Subtypes
Fecal incontinence is often an unvoiced problem that causes significant social stigma. Approximately 2% of the US population suffers from fecal incontinence [28], with a higher prevalence among women and elderly persons. Several mechanisms are involved in the pathogenesis of fecal incontinence. A common cause is injury to the external or internal anal sphincter, puborectalis muscle, or pudendal nerves, often after obstetric trauma. Hence, a detailed obstetric history including number of vaginal deliveries, use of forceps, tears, and episiotomy is important. Sphincter disruption, most commonly after surgery for hemorrhoid or anal fissure, can result in incontinence. Likewise, reduced rectal compliance causes urgency and fecal incontinence. Impaired rectal sensation results in the accumulation of stool and overflow. Patients rarely have a single cause, with 80% having more than one factor that leads to incontinence [29].
Clinically, fecal incontinence can be classified into 3 categories. Urge incontinence is characterized by the inability to control stool discharge despite active attempts to retain contents. These patients often have disruption or injury to the external anal sphincter. Fecal seepage is the involuntary discharge of less than 2 tablespoons of stool matter without awareness. Seepage can result from impaired rectal evacuation and dyssynergia. Often patients with seepage complain of incomplete evacuation. Passive incontinence refers to the involuntary discharge of stool contents without awareness. These patients often have underlying neuropathy and sphincter weakness [30,31].
What is the approach to evaluation and diagnosis?
Evaluation and Diagnosis
Physical examination of patients with fecal incontinence should include a detailed rectal examination, similar to the exam performed in patients who present with constipation. It should include perineal inspection for fissures, fistulae, and skin excoriation. The anocutaneous reflex should be checked along with the resting and squeeze sphincter tone and sphincter relaxation. Further investigations should focus on determining the underlying mechanism in order to facilitate treatment.
Endoscopic investigation should be performed to exclude mucosal disease or malignancy. Anorectal manometry provides objective information regarding resting and squeeze anal sphincter tone, rectal compliance, rectal sensitivity, and rectoanal reflexes [29]. Some experts believe that anorectal manometry is not needed for diagnosis and emphasize the importance of rectal examination and history [32]. Proponents of anorectal manometry point out the importance of physiologic data that can be gained and how it may direct therapy. For example, anorectal manometry and sensory testing may reveal weak anal sphincters and impaired rectal sensation. The latter cannot be identified by clinical evaluation alone. These 2 pathophysiologic findings could enable the biofeedback therapist to focus on improving both anal sphincter tone and rectal sensation [33]. Defecography may reveal anterior rectocele, mucosal intussusception, or rectal prolapse. Anal ultrasound provides information on the structural integrity of the external and internal anal sphincters [34]. Ultrasound is widely available and is relatively inexpensive. Endoanal MRI may provide better information regarding the integrity of the external anal sphincter [35].
What are the treatment options?
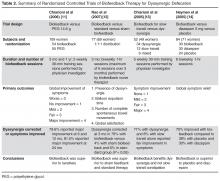
The goal of treatment is to restore continence and quality of life. General considerations include stool bulking agents such as fiber supplements. Antidiarrheal agents, such as loperamide and diphenoxylate/atropine, are useful as they can decrease stool volume and increase and prolong sphincter pressure and colonic transit time [36,37]. Patients with diarrhea and functional incontinence may benefit from treatment with cholestyramine [38]. Biofeedback therapy improves sphincter tone and rectal sensation [39]. The number of biofeedback sessions is titrated to the patient’s needs, but often 6 sessions are required [40]. Generally, a 70% success rate has been described. Table 4 summarizes recent evidence supporting the use of biofeedback in the treatment of fecal incontinence [41–46].
Surgery for incontinence should be reserved for patients who have failed aggressive conservative management and biofeedback therapy. Overlapping sphincteroplasty is the most common surgery performed for fecal incontinence, with a success rate between 35% and 70% [47,48]. Creation of a neosphincter via dynamic graciloplasty or artificial sphincter has been tried in patients with an irreversibly damaged anal sphincter, but the success rate is low and the complication rate is high [49].
Sacral nerve stimulation (SNS) involves inserting electrodes in the lower back and connecting them to a pulse generator that produces pulses of electricity that innervate the nerves controlling the anal sphincters. Two double-blind crossover studies have reported a beneficial effect of SNS in fecal incontinence [50,51]. In 19 patients who preferred the periods when the stimulator was turned on, the median number of fecal incontinence episodes per week decreased from 1.7 to 0.7, and in the 5 patients who preferred the off period, the median number of fecal incontinence episodes per week increased from 1.7 to 3.7. SNS is now approved by FDA and insurance payers. Recently, hyaluronic acid/dextranomer injection (Solesta, Salix Pharmaceuticals, Raleigh, NC) has also been approved by FDA and has been shown to improve incontinence. A randomized controlled trial showed a 52% response rate to hyaluronic acid/dextranomer compared to a 31% response with placebo [52].
Conclusion
The 3 cases presented illustrate the complexities of several common anorectal disorders. A definitive diagnosis can be established in patients with defecation disorders through systematic evaluations and physiologic and imaging studies. Diagnosis in turn can pave the way for appropriate medical, behavioral, or surgical treatment. If facilities for appropriate testing are unavailable, it is important to refer these patients to appropriate specialists instead of embarking on empirical therapies which may prove futile. Treatment is often possible, and in a majority of patients their symptoms can be ameliorated.
Corresponding author: Satish S.C. Rao, MD, PhD, Section of Gastroenterology and Hepatology, Medical College of Georgia, Georgia Regents University, BB R2540, 1120 15th St., Augusta, GA 30912.
Funding/support: Portions of this work were supported by National Institutes of Health grant RO1 DK 57100-05.