IBS: Mental Health Factors and Comorbidities





Lin Chang, MD
Professor, David Geffen School of Medicine,
UCLA; Vice-Chief, Vatche and Tamar
Manoukian, Division of Digestive Diseases,
UCLA Digestive Diseases Center,
Los Angeles, California
Disclosures: Serve(d) as a director, officer, partner, employee, advisor,
consultant, or trustee for: Ardelyx; Alfasigma; Atmo; GLaxoSmithKline;
Food Marble; Vibrant; Nerva; Received research grant from: AnX Robotica;
Ironwood; Received income in an amount equal to or greater than $250
from: Alfasigma; Atmo; GLaxoSmithKline; Food Marble; Have stock options
in: Trellus Health; Food Marble; ModifyHealth
Laurie A. Keefer, PhD
Professor, Department of Medicine and
Psychiatry, Division of Gastroenterology, Icahn
School of Medicine at Mount Sinai; Gastro
Psychologist, Inflammatory Bowel Disease Center,
Mount Sinai Hospital, New York, New York
Disclosures: Serve(d) as a director, officer, partner, employee, advisor,
consultant, or trustee for: AbbVie; Pfizer; Eli Lilly; Reckitt Health; Johnson
and Johnson; Rome Foundation; Received research grant from: Ardelyx
Have a 5% or greater equity interest in: Trellus Health





Irritable bowel syndrome (IBS), a disorder of gut-brain interaction, affects up to 10% of the global population.1 Psychological symptoms often are associated with IBS, increasing its burden and affecting quality of life.1-3 About one third of patients with IBS experience anxiety or depression.1 Multidisciplinary care, involving gastroenterologists, psychologists, and dietitians, is crucial to address both physical and emotional symptoms in patients with IBS.1
Effective clinical pathways vary by patient profile. Some patients may have maladaptive cognitive processes that affect coping with IBS (e.g., avoidance behaviors and symptom-related anxiety) but do not meet criteria for a psychiatric disorder.2 For these patients, referral to brain-gut behavior therapy (BGBT) is advised.2 BGBTs can include cognitive behavioral therapy (CBT), gut-directed hypnotherapy, and mindfulness-based interventions, among others.3 These approaches can improve not only mental health symptoms and symptom-related stress but also gastrointestinal (GI) symptoms.4 For patients with psychiatric illnesses, referrals to psychiatrists or psychologists specialized in the patient’s specific comorbid condition are recommended.2 It is also helpful for GI professionals to familiarize themselves with a few antidepressant medications for symptom-specific anxiety or mood symptoms when a psychiatrist is unavailable.5,6 Some antidepressants, called central neuromodulators, also improve IBS symptoms.5,6
Access to integrated IBS care remains a challenge. The number of GI psychologists is limited. Most digital applications aiming to bridge this gap have limitations, such as nonpersonalized approaches and problems with engagement.7 Other options to provide care for patients with IBS and psychological symptoms include support groups or nurse-led self-management programs, education, patient advocacy organizations, and placement of educational material in clinic waiting areas.3
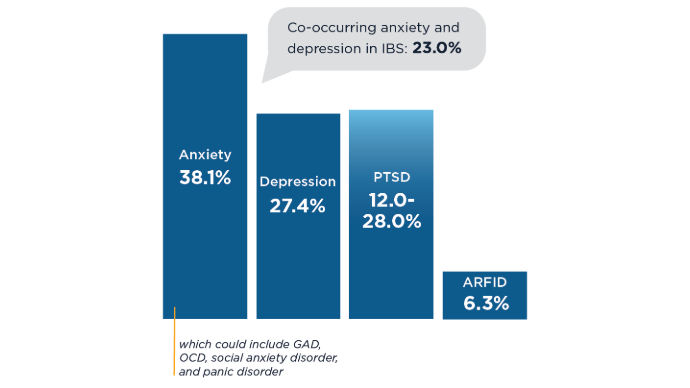 Prevalence of Mental Health Conditions in IBS1,8,9
Prevalence of Mental Health Conditions in IBS1,8,9
Many patients with IBS have comorbid mental health conditions, and many patients with mental health disorders have gut symptoms.1 This bidirectional relationship is attributed to shared biological pathways along the gut-brain axis.1 GI symptom-related anxiety is also common in IBS and is not the same as GAD. ARFID, avoidant restrictive food intake disorder; GAD, generalized anxiety disorder; OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder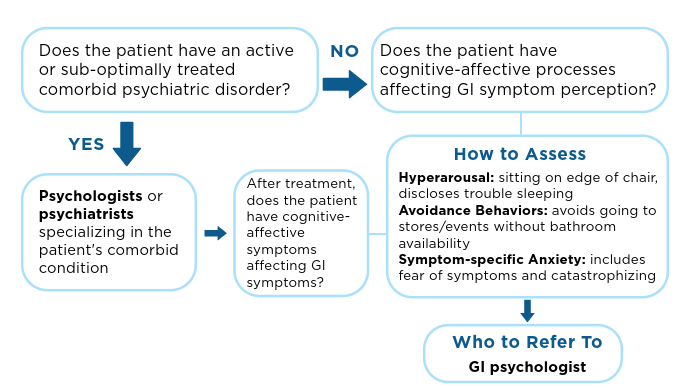 Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
Patients with IBS may have a comorbid psychiatric disorder and/or cognitive-affective symptoms related to GI symptoms.3 The clinician should assess which is the predominant issue.2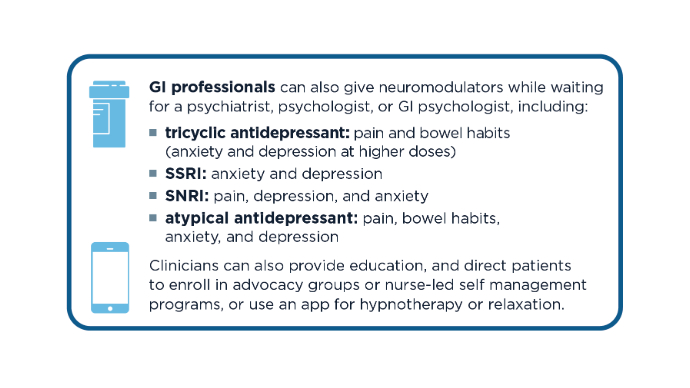 Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
The clinician can prescribe neuromodulators or antidepressants to treat IBS and mood if indicated.6 If the patient is seeing a psychiatrist, the clinician should work with the patient's psychiatrist about medication changes.6 SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin-norepinephrine reuptake inhibitor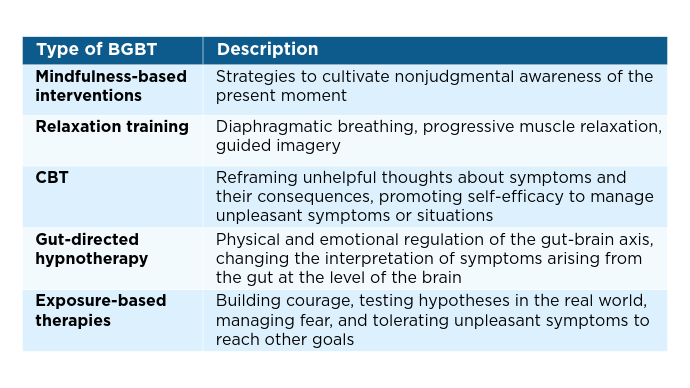 Types of BGBTs and Uses3,7
Types of BGBTs and Uses3,7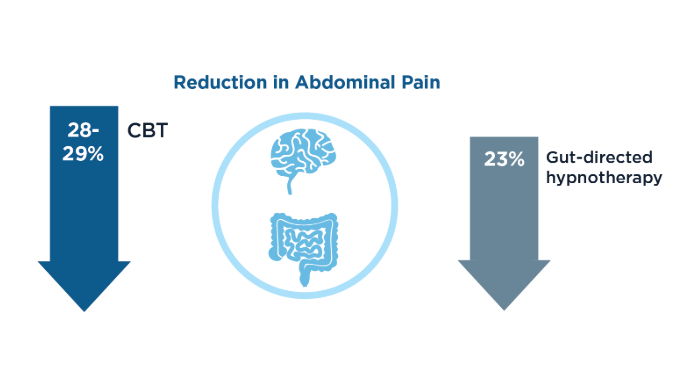 BGBT Effect on Abdominal Pain4
BGBT Effect on Abdominal Pain4
BGBT can address both mental health and GI symptoms. In a meta-analysis of 42 randomized controlled trials (RCTs) in IBS, BGBTs were associated with improvements in abdominal pain.4 BGBTs appear most effective for patients who accept their diagnosis, understand the gut-brain connection, and are motivated to change.4 For future RCTs, a suggested focus is an existing behavioral treatment development model that has iterative progression, as in the drug development model, and includes BGBT nuances.12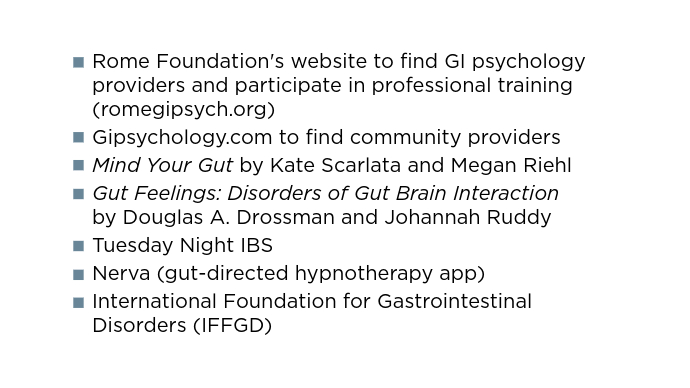 Resources for Patients and Providers13-18
Resources for Patients and Providers13-18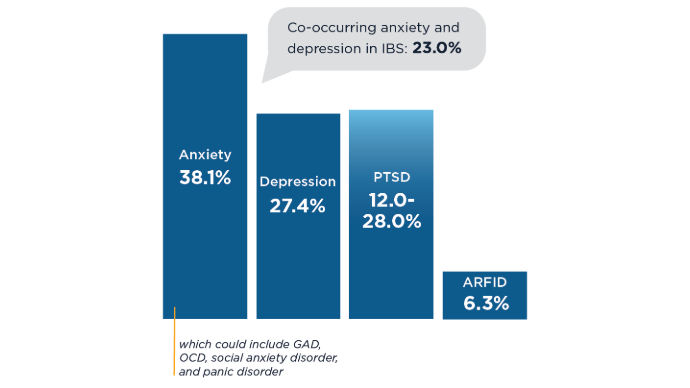 Prevalence of Mental Health Conditions in IBS1,8,9
Prevalence of Mental Health Conditions in IBS1,8,9
Many patients with IBS have comorbid mental health conditions, and many patients with mental health disorders have gut symptoms.1 This bidirectional relationship is attributed to shared biological pathways along the gut-brain axis.1 GI symptom-related anxiety is also common in IBS and is not the same as GAD. ARFID, avoidant restrictive food intake disorder; GAD, generalized anxiety disorder; OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder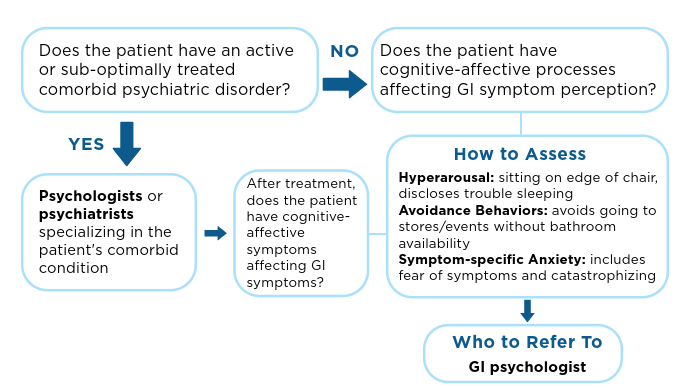 Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
Patients with IBS may have a comorbid psychiatric disorder and/or cognitive-affective symptoms related to GI symptoms.3 The clinician should assess which is the predominant issue.2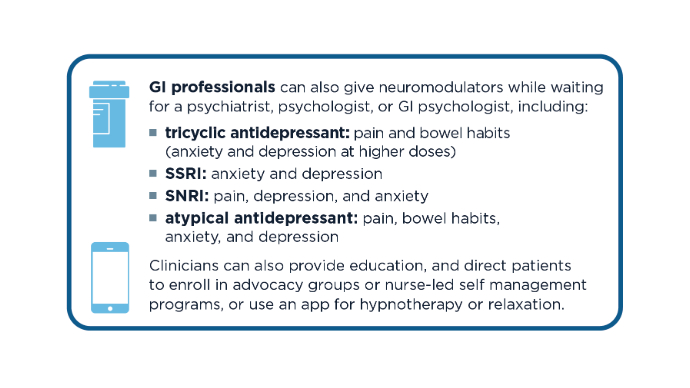 Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
The clinician can prescribe neuromodulators or antidepressants to treat IBS and mood if indicated.6 If the patient is seeing a psychiatrist, the clinician should work with the patient's psychiatrist about medication changes.6 SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin-norepinephrine reuptake inhibitor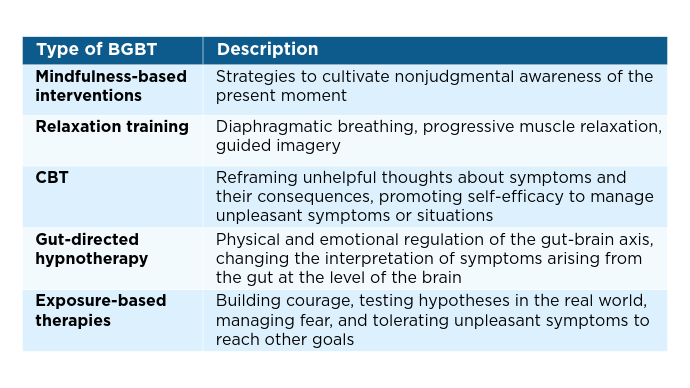 Types of BGBTs and Uses3,7
Types of BGBTs and Uses3,7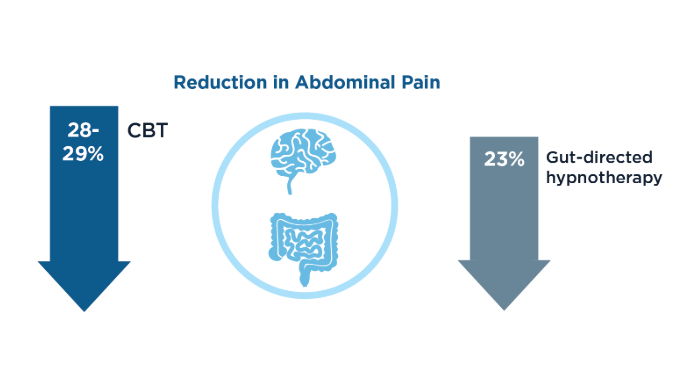 BGBT Effect on Abdominal Pain4
BGBT Effect on Abdominal Pain4
BGBT can address both mental health and GI symptoms. In a meta-analysis of 42 randomized controlled trials (RCTs) in IBS, BGBTs were associated with improvements in abdominal pain.4 BGBTs appear most effective for patients who accept their diagnosis, understand the gut-brain connection, and are motivated to change.4 For future RCTs, a suggested focus is an existing behavioral treatment development model that has iterative progression, as in the drug development model, and includes BGBT nuances.12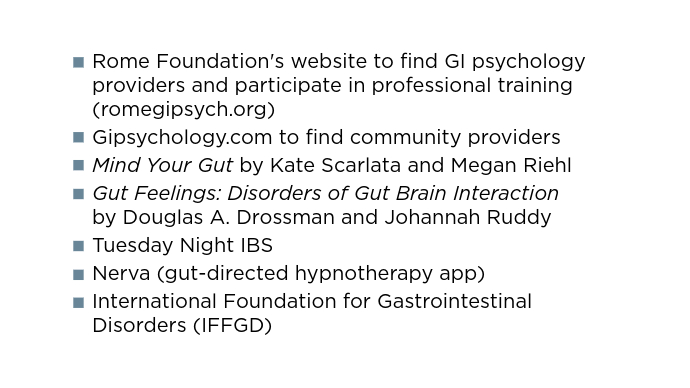 Resources for Patients and Providers13-18
Resources for Patients and Providers13-18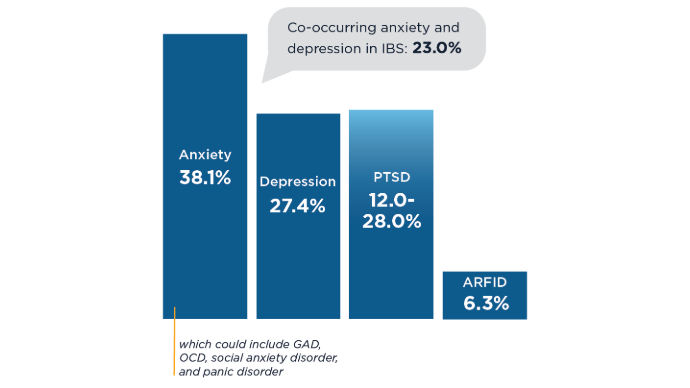 Prevalence of Mental Health Conditions in IBS1,8,9
Prevalence of Mental Health Conditions in IBS1,8,9
Many patients with IBS have comorbid mental health conditions, and many patients with mental health disorders have gut symptoms.1 This bidirectional relationship is attributed to shared biological pathways along the gut-brain axis.1 GI symptom-related anxiety is also common in IBS and is not the same as GAD. ARFID, avoidant restrictive food intake disorder; GAD, generalized anxiety disorder; OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder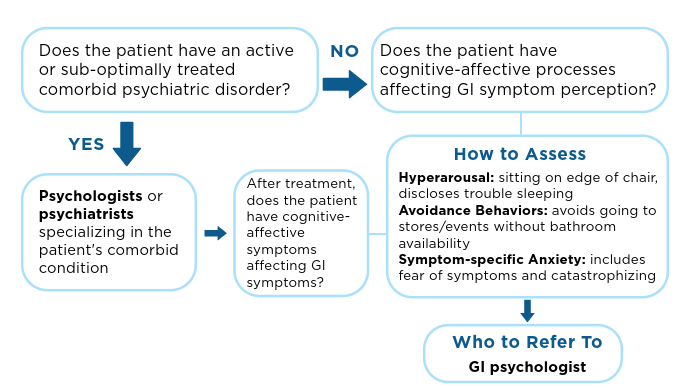 Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
Patients with IBS may have a comorbid psychiatric disorder and/or cognitive-affective symptoms related to GI symptoms.3 The clinician should assess which is the predominant issue.2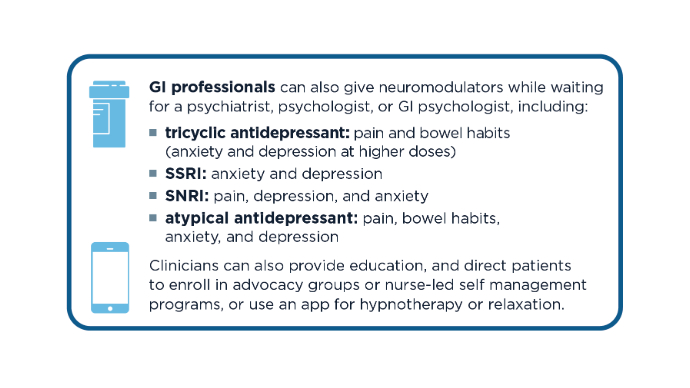 Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
Treatment Framework for IBS With Mental Health Features1-3,6,7,10,11
The clinician can prescribe neuromodulators or antidepressants to treat IBS and mood if indicated.6 If the patient is seeing a psychiatrist, the clinician should work with the patient's psychiatrist about medication changes.6 SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin-norepinephrine reuptake inhibitor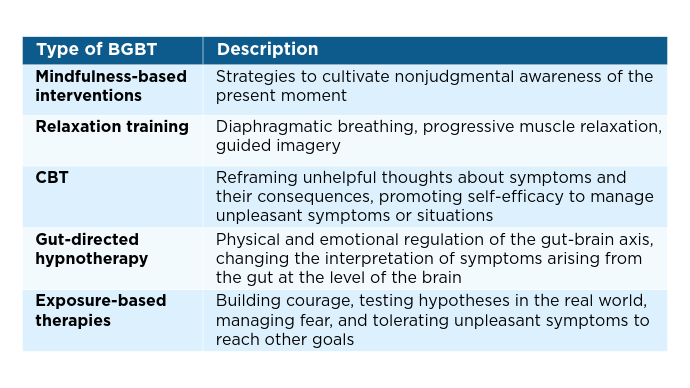 Types of BGBTs and Uses3,7
Types of BGBTs and Uses3,7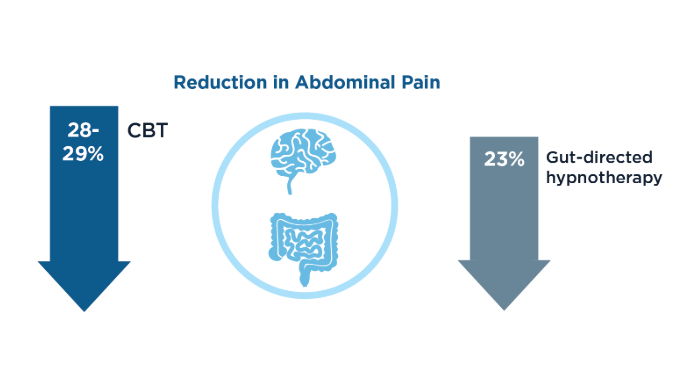 BGBT Effect on Abdominal Pain4
BGBT Effect on Abdominal Pain4
BGBT can address both mental health and GI symptoms. In a meta-analysis of 42 randomized controlled trials (RCTs) in IBS, BGBTs were associated with improvements in abdominal pain.4 BGBTs appear most effective for patients who accept their diagnosis, understand the gut-brain connection, and are motivated to change.4 For future RCTs, a suggested focus is an existing behavioral treatment development model that has iterative progression, as in the drug development model, and includes BGBT nuances.12 Resources for Patients and Providers13-18
Resources for Patients and Providers13-18
Click to view more from Gastroenterology Data Trends 2025.
,false
