Achalasia Remains a Challenging Disorder for the Community Gastroenterologist










Considerable advances in our understanding of esophageal achalasia have been made in the 21st century, accompanied by new diagnostic and treatment modalities. Indeed, about half of the available citations for the term achalasia in PubMed have been published in the past 20 years.1 These developments have increased awareness of this condition among practicing gastroenterologists. But because achalasia is a rare disorder in which the available treatments are palliative, it continues to present a challenge for the community gastroenterologist to diagnose and manage.2
The first problem for diagnosis concerns the rarity of the condition combined with lack of specificity of the presenting symptoms, particularly early in the disease course. Because the prevalence of troublesome GERD (18,000/100,000) is easily 1,000-fold greater than that of achalasia (just 15/100,000), a patient presenting anew with any constellation of esophageal symptoms is far more likely to have them result from GERD than achalasia.3,4 Further, the classic features of achalasia—massive esophageal dilation with retained contents—are often absent on endoscopic or radiographic evaluation early in the disease.
When initial testing shows no findings confirming a GERD diagnosis and symptoms fail to respond to GERD therapy, or testing identifies late-stage morphologic features suggesting an achalasia diagnosis, the next step in evaluation is esophageal high-resolution manometry (HRM). This test is currently the standard of care for an achalasia diagnosis.5 Community gastroenterologists are increasingly incorporating HRM into their practice, and likely discovering that the learning curve for generating high-quality studies and accurate interpretations of HRM findings is steep, particularly if they have had no training with this technology during their fellowship.6-8
The findings on HRM are characterized into 3 different motor phenotypes, per the Chicago Classification, which have implications for treatment approach and prognosis. Manometric findings always must be considered within the context of the patient’s entire clinical picture, to avoid misdiagnosis of achalasia and subsequent inappropriate treatment decisions. Other diagnoses, such as opiate-induced dysmotility, “pseudoachalasia” due to cancers, and end-stage esophageal dysfunction in systemic sclerosis, can have findings on HRM that mimic those of idiopathic achalasia.9-11
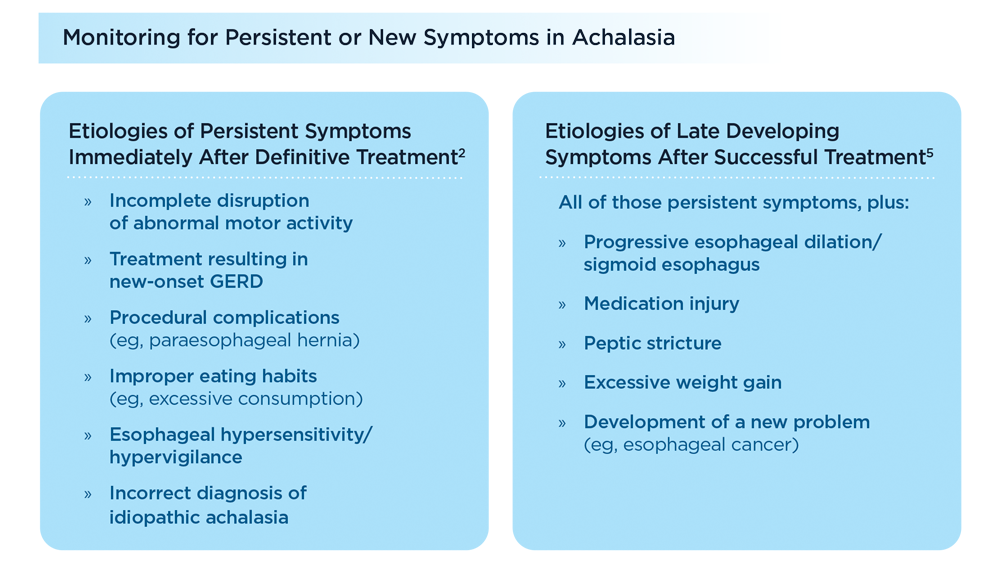
All definitive treatments for idiopathic achalasia (pneumatic dilation, laparoscopic myotomy, peroral endoscopic myotomy [POEM]) have the goal of irreversibly disrupting abnormal smooth muscle function causing outflow obstruction at the esophageal outlet or spastic contractions in the esophageal body. When applied to the appropriate achalasia motor phenotype, all offer reasonable palliation of symptoms in most, but not all, patients, with a small but immediate risk of serious complications.2 The best choice often depends on the degree of locally available expertise for the different treatment options, which in the case of pneumatic dilation is unfortunately declining in the United States. While increasing percentages of patients are being treated with POEM, the high rate of postprocedure reflux has uncertain implications for these patients in the future.2
Because no treatment can return esophagus function to normal, patients require ongoing follow-up to monito for signs and symptoms of disease progression or new complications. Patients need to be counseled regarding the risks of esophageal pill injury, imprudent eating habits (eg, excessive consumption), excessive weight gain, and neglecting new-onset GERD symptoms.
Click to view more from Gastroenterology Data Trends 2022.
,false