Medication-Nonadherent Hypothyroidism Requiring Frequent Primary Care Visits to Achieve Euthyroidism
Background: Nonadherence to medications is a common clinical issue. We describe a case in which weekly visits to assess medication adherence achieved euthyroidism in a patient with persistent primary hypothyroidism and suspected nonadherence to levothyroxine. The patient, however, did not report nonadherence.
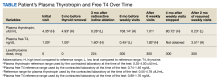
Case Presentation: A male aged 67 years with multinodular goiter underwent total thyroidectomy for abnormal thyroid nodule biopsy. Surgical pathology revealed papillary thyroid cancer with lymph node metastasis for which he received radioactive iodine treatment. His plasma thyrotropin (TSH) was noted to be 0.28 uIU/mL (reference range 0.35-4.00 uIU/mL) 7 months postsurgery while taking 224 mcg levothyroxine tablets daily. His plasma TSH remained elevated for about 5 years despite titrations of the levothyroxine dosage, counseling, and multiple follow-up visits. A home care nurse was involved in monitoring the patient taking levothyroxine daily and correctly but was unsuccessful. The patient and his son reported taking levothyroxine daily and correctly. The patient was asked to visit the primary care clinic every week for 6 weeks with all his medications. Repeat plasma TSH normalized to 1.01 uIU/mL. The suspected etiology of previously high plasma TSH was nonadherence to levothyroxine, which was discussed in detail with the patient. The patient verbalized understanding, was willing to follow recommendations and ended the weekly clinic visits. Repeat plasma TSH was again high and the patient claimed adherence, but weekly visits to primary care clinic were resumed, and life-threatening consequences of hypothyroidism were discussed with the patient and his son. After 9 weeks of visits, he was noted to have low plasma TSH (0.23 uIU/mL).
Conclusions: Weekly visits seem impractical but may help in cases of persistent hypothyroidism in which the patient admits to being or is suspected to be nonadherent to levothyroxine. Knowing their medication use will be checked at weekly clinic visits may motivate the patient to be adherent.
Nonadherence to medications is an issue across health care. In endocrinology, hypothyroidism, a deficiency of thyroid hormones, is most often treated with levothyroxine and if left untreated can lead to myxedema coma, which can lead to death due to multiorgan dysfunction.1 Therefore, adherence to levothyroxine is very important in preventing fatal complications.
We present the case of a patient with persistent primary hypothyroidism who was suspected to be nonadherent to levothyroxine, although the patient consistently claimed adherence. The patient’s plasma thyrotropin (TSH) level improved to reference range after 6 weeks of weekly primary care clinic visits. After stopping the visits, his plasma TSH level increased again, so 9 more weeks of visits resumed, which again helped bring down his plasma TSH levels.
Case Presentation
A male patient aged 67 years presented to the Dayton Veterans Affairs Medical Center (VAMC) endocrinology clinic for evaluation of thyroid nodules. The patient reported no history of neck irradiation and a physical examination was unremarkable. At that time, laboratory results showed a slightly elevated plasma TSH level of 4.35 uIU/mL (reference range, 0.35-4.00 uIU/mL) and normal free thyroxine (T4) of 1.00 ng/dL (reference range, 0.74-1.46 ng/dL). Later that year, the patient underwent a total thyroidectomy at the Cincinnati VAMC for Hurthle cell variant papillary thyroid carcinoma that was noted on biopsy at the Dayton VAMC. After surgical pathology results were available, the patient started levothyroxine 200 mcg daily, although 224 mcg would have been more appropriate based on his 142 kg weight. Due to a history of arrhythmia, the goal plasma TSH level was 0.10 to 0.50 uIU/mL. The patient subsequently underwent radioactive iodine ablation. After levothyroxine dose adjustments, the patient’s plasma TSH level was noted to be within his target range at 0.28 uIU/mL 3 months postablation.
Over the next 5 years the patient had regular laboratory tests during which his plasma TSH level rose and were typically high despite adjusting levothyroxine doses between 200 mcg and 325 mcg. The patient received counseling on taking the medication in the morning on an empty stomach and waiting at least 1 hour before consuming anything, and he went to many follow-up visits at the Dayton VAMC endocrinology clinic. He reported no vomiting or diarrhea but endorsed weight gain once. The patient also had high free T4 at times and did not take extra levothyroxine before undergoing laboratory tests.
Nonadherence to levothyroxine was suspected, but the patient insisted he was adherent. He received the medication in the mail regularly, generally had 90-day refills unless a dose change was made, used a pill box, and had social support from his son, but he did not use a phone alarm to remind him to take it. A home care nurse made weekly visits to make sure the remaining levothyroxine pill counts were correct; however, the patient continued to have difficulty maintaining daily adherence at home as indicated by the nurse’s pill counts not aligning with the number of pills which should have been left if the patient was talking the pills daily.
The patient was asked to visit a local community-based outpatient clinic (CBOC) weekly (to avoid patient travel time to Dayton VAMC > 1 hour) to check pill counts and assess adherence. The patient went to the CBOC clinic for these visits, during which pill counts indicated much better but not 100% adherence. After 6 weeks of clinic visits, his plasma TSH decreased to 1.01 uIU/mL, which was within the reference range, and the patient stopped coming to the weekly clinic visits (Table). Four months later, the patient's plasma TSH levels increased to 80.72 uIU/mL. Nonadherence to levothyroxine was suspected again. He was asked to resume weekly clinic visits, and the life-threatening effects of hypothyroidism and not taking levothyroxine were discussed with the patient and his son. The patient made CBOC clinic visits for 9 weeks, after which his plasma TSH level was low at 0.23 uIU/mL.