How Low Is Too Low? A Retrospective Analysis of Very Low LDL-C Levels in Veterans
Background: Low-density lipoprotein cholesterol (LDL-C) can build up on the walls of blood vessels, leading to coronary heart disease. Medications used to lower LDL-C levels have demonstrated decreased risks of atherosclerotic cardiovascular disease, but currently, there is no consensus on how to define very low LDL-C levels. It is necessary for the body to have LDL-C to maintain proper brain function; however, the safety and effects of prolonged very low LDL-C levels are unknown. The current study sought to gather information to determine the risks of very low LDL-C levels in a veteran population.
Methods: A retrospective chart review was conducted at a US Department of Veterans Affairs medical center. Patients with hyperlipidemia/dyslipidemia treated with HMG-CoA reductase inhibitors or proprotein convertase subtilisin/kexin type 9 (PCSK9) therapy and LDL-C levels < 40 mg/dL between January 1, 2010, and September 1, 2020, were included. The primary outcome was the rate of intracranial hemorrhage that could be caused by an LDL-C level < 40 mg/dL. The secondary outcomes included actions taken by clinicians, adverse drug reactions (ADRs), duration of therapy, and medication adherence.
Results: This study included 3027 patients. Of the included patients, 8 had an intracranial hemorrhage within 1 year from a documented LDL-C level < 40 mg/dL (0.26%). Thirty-two patients with an LDL-C level < 40 mg/dL did not have a documented ADR with the studied medications. Of the 32 charts, 26 had a clinician address the LDL-C level < 40 mg/dL with either documentation and/or modification of the medication prescribed. The most common ADRs among the studied medications were muscle and joint pain, rash, and cramps. Adherence to the medications was consistently similar for all studied medications.
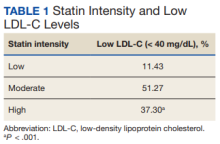
Conclusions: Of the patient population included in this study, 0.26% of patients had an intracranial hemorrhage within 1 year of having an LDL-C level < 40 mg/dL. The rate of ADRs related to the medications analyzed in this study shows no statistical significance ( P > .05). When compared with low- and moderate-intensity statin medications, high-intensity statin medications were statistically significant in resulting in an LDL-C level < 40 mg/dL ( P < .001). LDL-C levels < 40 mg/mL were not routinely documented as being addressed in the chart by the clinician.
Methods
A retrospective chart review was conducted on patients aged 18 to 90 years receiving care at the Hershel “Woody” Williams Veterans Affairs Medical Center (HWW VAMC) in Huntington, West Virginia, between January 1, 2010, and September 1, 2020. Approval of the current study was obtained through the Marshall University Institutional Review Board, HWW VAMC Research and Development Committee, and Veterans Health Administration (VHA) DATA Access Request Tracker (DART)/VA Informatic and Computing Infrastructure (VINCI). Data were obtained via the VHA Corporate Data Warehouse (CDW) for the HWW VAMC using Microsoft Structured Query Language (SQL) server available in VINCI. Analysis of the data was conducted using STATA v. 15.
Patients were included if they had a diagnosis of hyperlipidemia/dyslipidemia, received treatment with HMG-CoA reductase inhibitors or PCSK9 medications, and had an LDL-C level ≤ 40 mg/dL. The primary outcome was the rate of intracranial hemorrhage that could be caused by very low LDL-C levels. The secondary outcomes included actions taken by clinicians to address LDL-C level < 40 mg/dL, ADRs, duration of therapy, and medication adherence. Patients were excluded if they were aged < 18 or > 90 years, were pregnant during the study period, had hypothyroidism, received chronic anticoagulation medications, or had a triglyceride level > 300 mg/dL.
Results
The study included 3027 patients. Of those patients, 78 patients were female while 2949 were male, and the mean (SD) age was 68.3 (9.4) years. A subsample of 32 patients was analyzed to determine whether an ADR was noted or low LDL-C level was addressed in the chart. The subsample size was determined through chart review and included patients who had a documented intracranial hemorrhage. None of the 32 patients had an ADR documented, and 6 (19%) had the low LDL-C level addressed in the chart by monitoring levels, reducing statin doses, or discontinuing the medication. Of the total population analyzed, 8 patients (0.3%) had a documented intracranial hemorrhage within 1 year following the low LDL-C level.
We also analyzed the intensity of statin related to the low LDL-C level (Table 1).
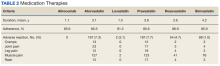
The most common ADRs were muscle, joint, and leg pain, rash, and cramps (Table 2).
Adherence to the medications and duration of therapy was also analyzed and was found to be similar among the various medications. Lovastatin had the highest percent adherence with 91.2% while atorvastatin had the lowest with 85.5%. It can be noted that lovastatin had a lower documented percentage of ADRs while atorvastatin had a higher documented percentage of ADRs, which can be clinically meaningful when prescribing these medications; however, these similar adherence rates are not influencing the primary outcome of the rate of intracranial hemorrhage due to LDL-C level < 40 mg/dL. Mean duration of therapy lasted between 1 year and > 4 years with 1.1 years for alirocumab and 4.2 for simvastatin. The duration of therapy could be influenced by formulary restrictions during the study time. Nonetheless, patients, regardless of formulary restrictions, have taken these medications for a duration long enough to affect LDL-C levels.