Assessment of Glucagon-like Peptide-1 Receptor Agonists in Veterans Taking Basal/Bolus Insulin Regimens
Background: Clinical use of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) is well established as add-on therapy to oral medications and basal insulin. However, there is little published data regarding the use of GLP-1 RAs for longer than 12 months in patients taking basal/bolus insulin regimens. The primary goal of our study was to assess the long-term efficacy of GLP-1 RAs as add-on therapy to basal/bolus insulin regimens.
Methods: This study was a retrospective record review of all patients on basal/bolus insulin regimens who received additional therapy with a GLP-1 RA. The primary outcome was the change in glycosylated hemoglobin A 1c (HbA 1c ) at 3, 6, 12, 18, and 24 months after initiation of the GLP-1 RA. Secondary outcomes included change in weight and total daily dose (TDD) of insulin and incidence of hypoglycemia and other adverse effects (AEs).
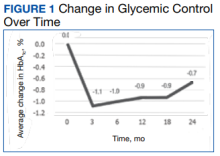
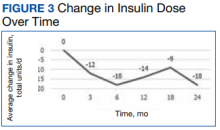
Results: Ninety-two patient records were reviewed. Mean glycemic control changed from baseline −1.1% (95% CI, −1.3 to −0.8; P < .001) at 3 months; −1.0% (95% CI, −1.3 to −0.7; P < .001) at 6 months; −0.9% (95% CI, 1.3 to −0.6; P < .001) at 12 months; −0.9% (95% CI, −1.4 to −0.3; P = .002) at 18 months; and −0.7 (95% CI, −1.4 to 0.1; P = .07) at 24 months. A significant decrease in weight was also observed from baseline through 18 months, and a significant decrease in TDD of insulin was identified from baseline through 12 months. Hypoglycemia was documented in 29.8% of patients at any point during GLP-1 RA therapy, and gastrointestinal AEs were documented in 18.3% of patients.
Conclusions: Adding GLP-1 RAs to complex insulin regimens may help achieve glycemic control while decreasing insulin requirements and mitigating undesirable AEs, such as weight gain.
Methods
This study was a retrospective, electronic health record review of all patients on basal and bolus insulin regimens who received additional therapy with a GLP-1 RA at Veteran Health Indiana in Indianapolis from September 1, 2015, to June 30, 2019. Patients meeting inclusion criteria served as their own control. The primary outcome was change in HbA1c at 3, 6, 12, 18, and 24 months after initiation of the GLP-1 RA. Secondary outcomes included change in weight and TDD of insulin at 3, 6, 12, 18, and 24 months after the initiation of the GLP-1 RAs and incidence of patient-reported or laboratory-confirmed hypoglycemia and other AEs.
Patients were included if they were aged ≥ 18 years with a diagnosis of T2DM, had concomitant prescriptions for both a basal insulin (glargine, detemir, or NPH) and a bolus insulin (aspart, lispro, or regular) before receiving add-on therapy with a GLP-1 RA (exenatide, liraglutide, albiglutide, lixisenatide, dulaglutide, or semaglutide) from September 1, 2015, to June 30, 2019, and had baseline and subsequent HbA1c measurements available in the electronic health record. Patients were excluded if they had a diagnosis of type 1 DM (T1DM), were followed by an outside clinician for DM care, or if the GLP-1 RA was discontinued before subsequent HbA1c measurement. The study protocol was approved by the Research and Development Office of Veteran Health Indiana, and the project was deemed exempt from review by the Indiana University Institutional Review Board due to the retrospective nature of the study.
Data analysis was performed using Excel. Change from baseline for each interval was computed, and 1 sample t tests (2-tailed) compared change from baseline to no change. Due to the disparity in the number of patients with data available at each of the time intervals, a mean plot was presented for each group of patients within each interval, allowing mean changes in individual groups to be observed over time.
Results
One hundred twenty-three subjects met inclusion criteria; 16 patients were excluded due to GLP-1 RA discontinuation before follow-up measurement of HbA1c; 14 were excluded due to patients being managed by a clinician outside of the facility; 1 patient was excluded for lack of documentation regarding baseline and subsequent insulin doses. Ninety-two patient charts were reviewed. Participants had a mean age of 64 years, 95% were male, and 89% were White. Mean baseline HbA1c was 9.2%, mean body mass index was 38.9, and the mean TDD of insulin was 184 units.
Since some patients switched between GLP-1 RAs throughout the study and there was variation in timing of laboratory and clinic follow-up,