Implementation of a Virtual Huddle to Support Patient Care During the COVID-19 Pandemic
Background: During a surge of COVID-19 cases, the volume of acute care patients with hypoxemic respiratory failure placed a high burden of responsibility on internal medicine, pulmonary and critical care medicine, and clinical pharmacy services.
Observations: We describe the COVID-19 Tele-Huddle Program, a novel approach to communication between key stakeholders in COVID-19 patient care through a daily video conferencing huddle. The program was implemented during a 4-week surge in COVID-19 cases at a large, academic medical center in Houston, Texas. Data collected during the COVID-19 Tele-Huddle Program included the type and number of interventions implemented, number of patients discussed, and COVID-19 therapies provided. In addition, hospital medicine team members completed a user-experience survey.
Conclusions: A multidisciplinary consultation service using video conferencing can support the care of patients with high disease severity without overwhelming existing inpatient medical, intensive care, and pharmacy services.
The COVID-19 pandemic challenged hospital medicine teams to care for patients with complex respiratory needs, comply with evolving protocols, and remain abreast of new therapies.1,2 Pulmonary and critical care medicine (PCCM) faculty grappled with similar issues, acknowledging that their critical care expertise could be beneficial outside of the intensive care unit (ICU). Clinical pharmacists managed the procurement, allocation, and monitoring of complex (and sometimes limited) pharmacologic therapies. Although strategies used by health care systems to prepare and restructure for COVID-19 are reported, processes to enhance multidisciplinary care are limited.3,4 Therefore, we developed the COVID-19 Tele-Huddle Program using video conference to support hospital medicine teams caring for patients with COVID-19 and high disease severity.
Program Description
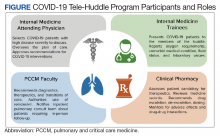
The Michael E. DeBakey Veterans Affairs Medical Center (MEDVAMC) in Houston, Texas, is a 349-bed, level 1A federal health care facility serving more than 113,000 veterans in southeast Texas.5 The COVID-19 Tele-Huddle Program took place over a 4-week period from July 6 to August 2, 2020. By the end of the 4-week period, there was a decline in the number of COVID patient admissions and thus the need for the huddle. Participation in the huddle also declined, likely reflecting the end of the surge and an increase in knowledge about COVID management acquired by the teams. Each COVID-19 Tele-Huddle Program consultation session consisted of at least 1 member from each hospital medicine team, 1 to 2 PCCM faculty members, and 1 to 2 clinical pharmacy specialists (Figure). The consultation team members included 4 PCCM faculty members and 2 clinical pharmacy specialists. The internal medicine (IM) participants included 10 ward teams with a total of 20 interns (PGY1), 12 upper-level residents (PGY2 and PGY 3), and 10 attending physicians.
The COVID-19 Tele-Huddle Program was a daily (including weekends) video conference. The hospital medicine team members joined the huddle from team workrooms, using webcams supplied by the MEDVAMC information technology department. The COVID-19 Tele-Huddle Program consultation team members joined remotely. Each hospital medicine team joined the huddle at a pre-assigned 15- to 30-minute time allotment, which varied based on patient volume. Participation in the huddle was mandatory for the first week and became optional thereafter. This was in recognition of the steep learning curve and provided the teams both basic knowledge of COVID management and a shared understanding of when a multidisciplinary consultation would be critical. Mandatory daily participation was challenging due to the pressures of patient volume during the surge.
COVID-19 patients with high disease severity were discussed during huddles based on specific criteria: all newly admitted COVID-19 patients, patients requiring step-down level of care, those with increasing oxygen requirements, and/or patients requiring authorization of remdesivir therapy, which required clinical pharmacy authorization at MEDVAMC. The hospital medicine teams reported the patients’ oxygen requirements, comorbid medical conditions, current and prior therapies, fluid status, and relevant laboratory values. A dashboard using the Premier Inc. TheraDoc clinical decision support system was developed to display patient vital signs, laboratory values, and medications. The PCCM faculty and clinical pharmacists listened to inpatient medicine teams presentations and used the dashboard and radiographic images to formulate clinical decisions. Discussion of a patient at the huddle did not preclude in-person consultation at any time.
Tele-Huddles were not recorded, and all protected health information discussed was accessed through the electronic health record using a secure network. Data on length of the meeting, number of patients discussed, and management decisions were recorded daily in a spreadsheet. At the end of the 4-week surge, participants in the program completed a survey, which assessed participant demographics, prior experience with COVID-19, and satisfaction with the program based on a series of agree/disagree questions.
Program Metrics
During the COVID-19 Tele-Huddle Program 4-week evaluation period, 323 encounters were discussed with 117 unique patients with COVID-19. A median (IQR) of 5 (4-8) hospital medicine teams discussed 15 (9-18) patients. The COVID-19 Tele-Huddle Program lasted a median (IQR) 74 (53-94) minutes. A mean (SD) 27% (13) of patients with COVID-19 admitted to the acute care services were discussed.
The multidisciplinary team provided 247 chest X-ray interpretations, 82 diagnostic recommendations, 206 therapeutic recommendations, and 32 transition of care recommendations (Table 1). A total of 55 (47%) patients were given remdesivir with first dose authorized by clinical pharmacy and given within a median (IQR) 6 (3-10) hours after the order was placed. Oxygen therapy, including titration and de-escalation of high-flow nasal cannula and noninvasive positive pressure ventilation (NIPPV), was used for 26 (22.2%) patients. Additional interventions included the review of imaging, the assessment of volume status to guide diuretic recommendations, and the discussion of goals of care.
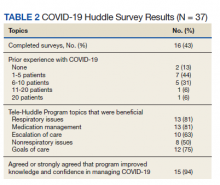
Of the participating IM trainees and attendings, 16 of 37 (43%) completed the user survey (Table 2). Prior experience with COVID-19 patients varied, with 7 of 16 respondents indicating experience with ≥ 5 patients with COVID-19 prior to the intervention period. Respondents believed that the huddle was helpful in management of respiratory issues (13 of 16), management of medications (13 of 16), escalation of care to ICU (10 of 16), and management of nonrespiratory issues (8 of 16) and goals of care (12 of 16). Fifteen of 16 participants strongly agreed or agreed that the COVID-19 Tele-Huddle Program improved their knowledge and confidence in managing patients. One participant commented, “Getting interdisciplinary help on COVID patients has really helped our team feel confident in our decisions about some of these very complex patients.” Another respondent commented, “Reliability was very helpful for planning how to discuss updates with our patients rather than the formal consultative process.”