Incidence of Chronic Opioid Use in Previously Opioid-Naïve Patients Receiving Opioids for Analgesia in the Intensive Care Unit
Objective: Inappropriate prescribing of opioids has contributed to misuse and a rise in accidental deaths. The purpose of this study was to determine the incidence of chronic opioid use in previously opioid-naïve patients who received opioids for analgesia while in the intensive care unit (ICU) and to identify potential risk factors in patients that transition to chronic opioid use.
Methods: A retrospective analysis included patients admitted to the medical, surgical, or cardiovascular ICU at the Michael E. DeBakey VA Medical Center in Houston, Texas, between August 2017 and December 2017. Patients were screened to confirm opioid-naïve status prior to admission, defined as ≤ 30 days of opioid prescription use in the prior 12 months. Patients were included if they received a continuous opioid infusion for ≥ 12 consecutive hours. Prescription fill data from the health record were examined at 3, 6, and 12 months postdischarge to determine whether patients were receiving chronic opioid treatment.
Results: Records of 330 patients were reviewed and 118 patients met the inclusion criteria. All patients received fentanyl infusion, for a median time of 35 hours (interquartile range 18.8-64.7 hours). Ninety (76.3%) patients were receiving opioids postdischarge at 3 months, 23 (19.5%) at 6 months, and 9 (7.6%) at 12 months. At 3 months, ICU type (odds ratio [OR], 3.9; 95% CI 1.73-8.75; P < .001) and being a surgical patient (OR, 7.8; 95% CI 3.26-18.56; P < .001) were risk factors for chronic opioid use. No specific risk factors were found to increase the risk of chronic opioid use at 6 and 12 months.
Conclusions: The incidence of chronic opioid use decreased at 6 and 12 months compared with that of 3 months postdischarge. ICU type and hospital admission related to surgery were not associated with increased opioid use at 3 months.
Methods
This analysis was a single center, retrospective chart review conducted for patients admitted between July 1, 2017 and December 31, 2017 at the US Department of Veterans Affairs (VA) Michael E. DeBakey VA Medical Center (MEDVAMC) in Houston, Texas. MEDVAMC is a 538-bed academic\teaching hospital serving about 130,000 veterans in Southeast Texas. The hospital has 3 ICUs (medical, cardiovascular, and surgical) and 38 total ICU beds. The study was approved by the Baylor College of Medicine Institutional Review Board and MEDVAMC Research and Development Review Board. Informed consent was not required.
Inclusion criteria consisted of patients aged ≥ 18 years admitted to the ICU in the above-specified time frame, who were administered a continuous infusion of an opioid for at least 12 hours. Patients were excluded if they were not opioid naïve prior to admission, defined as receiving > 30 days of opioids in the prior 12 months. Patients who died during hospital admission, never received an opioid despite having an active order, were hospital-to-hospital transfers, or were still admitted at the time of data collection were excluded from the analysis.
All pertinent data were collected using the VA Computerized Patient Record System (CPRS) and the Critical Care Manager (Picis Clinical Solutions) ICU monitoring application. Critical Care Manager was used to track the time frame, duration, and amounts of opioid infusions administered in the ICU. Patient demographic and preadmission data, including date of birth, age, race, history of substance use/alcohol use disorder (defined as a previous diagnosis) and previous opioid prescriptions within the past year were recorded. For the inpatient admission, the ICU LOS, hospital LOS, primary admission diagnosis, type of opioid medication administered, and total duration and dose of opioid administered were collected. After discharge, opioid medication fill data at 3, 6, and 12 months were collected. This information included names of any outpatient opioids filled, dosage unit, quantity, day supply, and number of refills.
The primary outcome for this study was to determine the incidence of chronic opioid use at 3, 6, and 12 months after discharge, defined as the percentage of patients receiving outpatient opioid prescriptions at each time point. Analyses were conducted to observe the effect of age, race, history of substance use or history of alcohol use (International Classification of Diseases documented diagnosis, 9th edition), ICU type (medical, surgical, or cardiovascular), surgical/nonsurgical admission, ICU LOS, hospital LOS, total time, and amount of opioids administered during admission on risk of conversion to chronic opioid use.
Descriptive statistics were calculated to analyze the incidence of chronic opioid use. Univariate logistic regression analysis, including ORs, 95% CIs, and P values, was conducted to determine the effects of the risk factors noted earlier on chronic opioid use at each time point. A multivariate logistic regression model was performed to assess the effect of multiple independent variables on opioid use at 3, 6, and 12 months. Statistical analysis was performed using StataCorp Stata SE.
Results
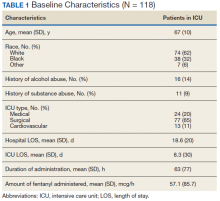
During the study period, 330 patients were admitted to the ICU. After applying inclusion/exclusion criteria, 118 patients were included in the final analysis. The most frequent reasons for exclusion from the study were patient death (n = 77), a past history of opioid use (n = 56), and not having received an opioid infusion for at least 12 hours (n = 68). The average age of the patients included was 67 years (Table 1). A total of 14% and 9% of patients, respectively, had a diagnosis of alcohol use disorder or substance use disorder recorded in CPRS. After admission, the most common location for these patients was the surgical ICU (65%). All patients were male. The average hospital LOS was 18.6 days , and the ICU LOS was 8.3 days. The average duration of administration for the opioid (fentanyl) infusion was 63 hours, and the average amount of fentanyl administered to each patient was 57.1 mcg/h.