Anesthesia Care Practice Models in the Veterans Health Administration
Statistical Analysis
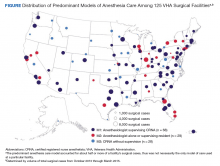
The percentage of surgical cases in each anesthesia care model was calculated overall and by the following characteristics: surgical case complexity, ASA classification, and facility complexity. The anesthesia model was determined for each case and summed at the facility level, yielding a total number of cases attributed to each model for each facility, thus identifying the predominant anesthesia model for each facility. The facilities were geographically displayed by their predominant anesthesia model and total number of surgical cases during the period. Because the aim was to present a descriptive representation of anesthesia care models, rather than infer significance, statistical testing was not included.
Results
A total of 484,082 surgical cases met inclusion criteria (Table). These cases were from 109 inpatient facilities and 16 ambulatory surgery facilities.
The percentage of cases in Model 1 was similar across the levels of surgical case complexity. However, a higher proportion of highly complex cases had a physician anesthesiologist (Model 2, 38.8%) than a CRNA (Model 3, 6.4%) as the primary anesthesia provider. Patients in each ASA classification were most likely to receive anesthesia care via Model 1. As ASA level increased, fewer patients had their anesthesia managed by a CRNA without supervision (Model 3: 18.4% of ASA 1 patients vs 8.3% of ASA 4 patients).
Facility complexity demonstrated notable differences in the proportions of surgical cases within each model. More than half of surgical cases in the largest, most complex facilities used Model 1 (64.9%, 58.2%, and 57.7% of cases in 1a, 1b, and 1c facilities, respectively). In comparison, Model 3 was found almost exclusively among surgical cases in smaller facilities with lower complexity (52% and 74% of cases in level 2 and 3 facilities, respectively).
The Figure displays the 125 facilities by their predominant model of anesthesia care. The diameter of the dots is relative to the facility’s total number of surgical cases. For each facility, the predominant model accounted for about half or more of cases but was not necessarily the only model of care used at a particular facility.
Related: Initiative to Minimize Pharmaceutical Risk in Older Veterans (IMPROVE) Polypharmacy Clinic
Discussion
Anesthesia care in more than half of surgical cases in VHA facilities was delivered by physician anesthesiologists supervising CRNAs. This model of anesthesia care was the dominant model in 54% of the facilities included in the sample. Consistent with a study of non-VHA facilities, this assessment found that the type of facility may influence the model of anesthesia care, with smaller, less complex facilities more often using a CRNA without supervision model.4 In these data, it was noted that among the 28 facilities that predominantly used Model 3, half had 12% or fewer cases that indicated a physician anesthesiologist model of care, and 6 had no cases with physician anesthesiologist involvement. These findings may reflect the limited scope of surgical services offered at lower complexity facilities and/or the reduced availability and/or utilization of physician anesthesiologists in these facilities.