A primary care guide to bipolar depression treatment
Manage uncomplicated cases following guidelines on medical therapy and with adjunctive psychotherapy. Refer complicated and severe cases to Psychiatry.
PRACTICE RECOMMENDATIONS
› Become knowledgeable in identifying an episode of bipolar depression and differentiating it from major depressive disorder, so as to provide effective treatment for bipolar depression. A
› Begin treatment of bipolar depression with one of the recommended first-line medications, especially lithium, lamotrigine, quetiapine, or lurasidone. A
› Treat bipolar II depression similar to the way bipolar I depression is treated: primarily, using a mood stabilizer alone or, occasionally, using a mood stabilizer plus an antidepressant. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Depressive episodes in the bipolar disorders. Bipolar depression can be seen in the settings of both bipolar I and II disorders. When a patient presents with a manic episode, a history of depressive episodes is common (although not essential) to diagnose bipolar I; alternatively, a history of hypomania (but no prior mania) and depression is needed to make the diagnosis of bipolar II. The natural history of the bipolar disorders is therefore alternating manic and almost always depressive episodes (bipolar I) and alternating hypomanic and always depressive episodes (bipolar II).8
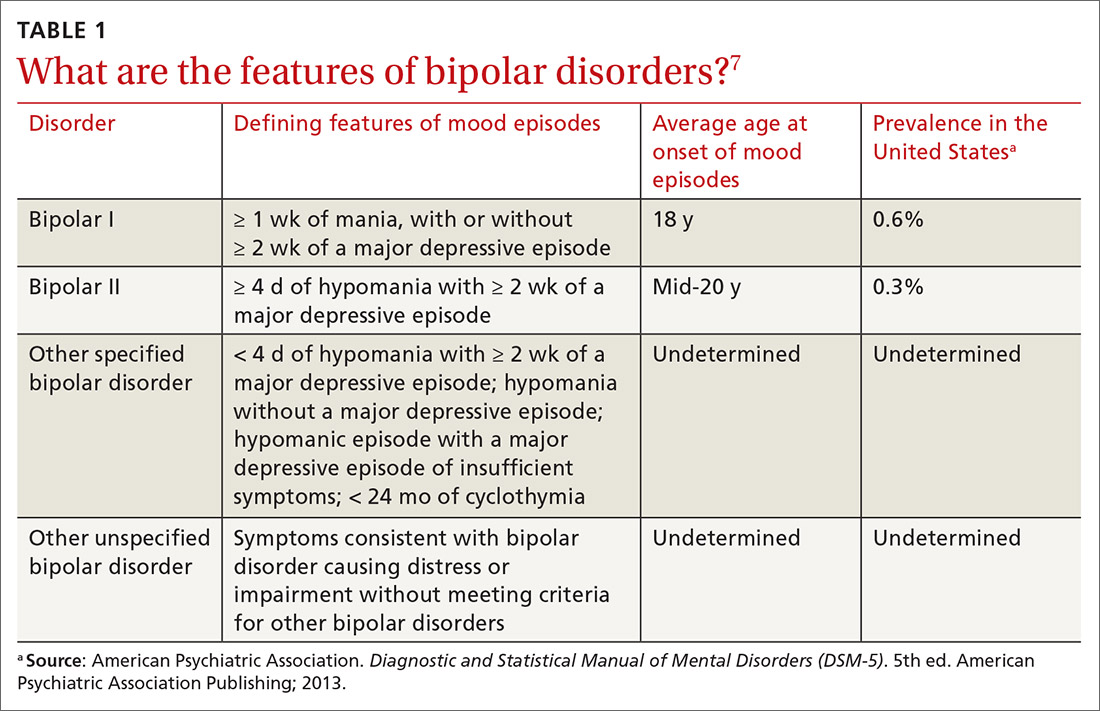
Symptoms of hypomanic episodes are similar to what are seen in manic episodes, but are of shorter duration (≥ 4 days [episodes of mania are at least of 1 week’s duration]), lower intensity (no psychotic symptoms), and not associated with significant functional impairment or hospitalization. Table 17 further describes the differentiating features of bipolar I and bipolar II. A history of an unequivocal manic or hypomanic episode makes the diagnosis of BD relatively easy. However, an unclear history of manic or hypomanic symptoms or episodes frequently leads to misdiagnosis or underdiagnosis of BD.
In both bipolar I and II, it is depressive symptoms and episodes that place the greatest burden on patients across the lifespan: They are the most commonly experienced features of the bipolar disorders9,10 and lead to significant distress and functional impairment11; in fact, patients with bipolar disorder spend 3 (or more) times as long in depressive episodes as in manic or hypomanic episodes.12,13 In addition, subthreshold depressive symptoms occur commonly between major mood episodes.
Failure to identify and adequately treat depressive episodes of the bipolar disorders can have serious consequences: Patients are at risk of a worsening course of illness, alcohol use disorder, substance use disorder, chronic disability, mixed states, rapid cycling of mood episodes, and suicide.
Guidelines for treating bipolar depression
Despite the similarity in presenting symptoms and signs of depressive episodes in bipolar disorders and MDD, treating episodes of BD is significantly different than treating MDD. Antidepressant monotherapy, a mainstay of treatment for MDD, has limited utility in BD (especially depressive episodes of bipolar I) because of its limited efficacy and potential to destabilize mood, lead to rapid cycling, and induce mania or hypomania. Treatment options for BD include pharmacotherapy (the primary modality), psychological intervention (a useful adjunct, described later), and electroconvulsive therapy (ECT; highly worth considering in severe or treatment-resistant cases).
Continue to: For this article...






