The Changing Landscape of Trauma Care, Part 2
Reaction Time. The R-time is measured in minutes and represents the time to clot initiation, reflecting activity of coagulation factors. It is used in TEG-guided MTPs to trigger transfusion of FFP.31,32 The R-time is measured at the time the clot strength reaches an amplitude of 2 mm.31 The angle reflects the rate of rise of the amplitude of the TEG tracing, or the rate of increase in clot strength. Clinically, the angle represents fibrinogen concentration and function, and is used to trigger transfusion of cryoprecipitate or fibrinogen concentrate in MTPs.31,32
Maximum Amplitude. The MA is reached by the TEG tracing, or the maximum clot strength achieved. Although the MA has been shown to correlate with platelet count, it actually represents platelet count and function as well as fibrinogen activity, all of which contribute to clot strength. Clinically, MA is used to trigger platelet transfusion and/or administration of desmopressin in MTPs.31,32
Lysis at 30 Minutes. The LY30 is defined as the percent reduction in clot strength 30 minutes after reaching MA.31,32 Normal LY30 values are between 0% and 7.5%; however, these values have been challenged in recent studies, which have reported that an LY30 greater than 3% (termed hyperfibrinolysis) confers a significant increase in mortality and an increased likelihood of requiring massive transfusion.31,33 These findings have led to incorporation of this lower threshold as a trigger for administration of TXA during MTPs. Furthermore, an LY30 of less than 0.8% (described as fibrinolysis shutdown) has also been found to confer an increase in mortality,34 which has led many to advocate for goal-directed administration of TXA, rather than empiric administration, as these patients are more likely to be harmed than helped by such an intervention.31
Rapid Thromboelastography
Rapid TEG employs tissue factor to accelerate clot initiation and reaction time, providing an additional parameter which reflects coagulation factor activity: the activated clotting time (ACT).32
Activated Clotting Time. Historically used in cardiac surgery to measure anticoagulation during a cardiopulmonary bypass, ACT represents the same phase of coagulation as R-time, but is measured in seconds instead of minutes.31 The ACT has been found to correlate with prothrombin time/international normalized ratio (PT/INR), and accurately predicts the need for MTP.
Cotton et al35 found that an ACT of more than 128 seconds predicted patients requiring MTP, and an ACT lower than 105 seconds predicted those who required no transfusions in the first 24 hours after injury.35
The ACT can be used to trigger transfusion of FFP, but at certain thresholds, may also be used to trigger the early transfusion of cryoprecipitate and platelets.36 Moore et al36 found that an ACT over 140 seconds was able to predict an abnormal angle and MA. This had led to using this threshold as a trigger for early administration of cryoprecipitate and platelets, given this parameter is available within 5 minutes—long before the angle and MA have resulted.
Efficacy
The use of a TEG-guided strategy for MTP in trauma has shown great promise. In 2013, Tapia et al37 compared a historical cohort who received 1:1:1 MTP to a TEG-guided MTP and demonstrated improved mortality.In 2016, Gonzalez et al38 compared TEG-guided transfusion vs conventional coagulation tests (PT/INR, PTT, fibrinogen, platelets). The authors found a significant decrease in mortality and platelet and FFP transfusion when TEG-guided resuscitation is used.
Endovascular Techniques
The use of endovascular techniques in trauma continues to evolve. According to the National Trauma Data Bank, the use of endovascular therapies has increased from 1% of trauma cases in 2002 to 11% in 2008.39
Thoracic Endovascular Aortic Repair
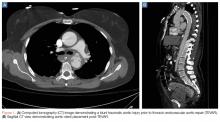
Thoracic endovascular aortic repair (TEVAR) for blunt thoracic aortic injury has essentially replaced open surgical repair. (See Figures 1a and 1b for an example of a blunt traumatic aortic injury prior to and post-TEVAR placement.)
Transarterial Catheter Embolization
Endovascular treatments have also been used successfully in the management of injuries to aortic branch vessels and extremity vessels.42 Transarterial catheter embolization with coils, plugs, or gel foam is being employed with increasing frequency to achieve hemostasis in the pelvis and spleen.42 It may also be used as an adjunct to laparotomy and perihepatic packing in high-grade liver injuries, though it is associated with significant morbidity related to hepatic necrosis, bile leaks, and abscesses.43,44
Resuscitative Endovascular Balloon Occlusion of the Aorta
Most recently, REBOA has been used for noncompressible torso hemorrhage following trauma. This method involves percutaneous arterial cannulation of the common femoral artery and advancement of a balloon into the aorta, where it is then inflated at the desired level.