Patient Safety in the Emergency Department
Patient safety has received increased attention since the late 1990s. In 1999, The Institute of Medicine published “To Err is Human: Building a Safer Health System,”1 followed by “Crossing the Quality Chasm: A New Health System for the 21st Century”2 in 2001 to document patient-safety issues and recommend improvements in medical care to reduce errors. These reports and other patient-safety studies, however, likely underestimate the extent of medical errors and preventable harm. After these reports appeared, many specialties began to seriously evaluate their own safety issues.
Among the specialties, emergency medicine (EM) identified several problem areas and attempted to determine the epidemiology of errors. One study of 62 urban EDs found that at least 7% of patients who presented for myocardial infarctions (MIs), asthma exacerbations, or joint dislocations requiring reduction with procedural sedation experienced an actual or near-miss adverse event.3 Another study showed that up to 12% of all return visits to the ED within 7 days were related to adverse events.4
The ED setting itself undoubtedly contributes significantly to the risk of harm. This article illustrates and discusses ED patient-safety issues, and offers some recommendations for improvement in care and prevention of harm.
The ED Setting
The ED is unlike any other area of the hospital or health-care setting. Patients seek care for both primary care and urgent care complaints at any time of the day or night, on any day of the week, when no other source of care is available. Emergency physicians (EPs) are required to care for multiple patients of different ages while prioritizing care of the critically ill who have MI, stroke, sepsis, respiratory distress, or multisystem trauma. For many ED patients, diagnosis and treatment can be complex.
The ED setting is fast-paced and requires quick thinking, a broad depth of knowledge about many medical conditions, and a broad range of skills to perform emergent and life-saving procedures. Often, patients are presenting to a hospital ED for the first time, with incomplete medical records. They may not know their medical conditions or medications, or be in a position to communicate this information. Any of these situations alone can lead to an adverse event; in combination, they can significantly increase the risk for harm. In addition, ED overcrowding due to limited availability of inpatient hospital beds may consume resources and staffing needed to care for active ED patients and new patients coming through the door.
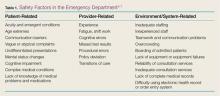
Safety factors in the ED can be categorized as those related to patients, providers, or the environment/systems (Table 1).5-7 When a large academic urban ED studied its errors, two-thirds were attributed to systems issues.5
Culture of Safety
Developing and maintaining a “culture of safety” is a commitment to minimize adverse events when performing high-risk jobs that can result in harm.8 This concept originated in other industries such as the airline and nuclear energy industries. Organizations and companies are considered high-reliability organizations (HROs) when they are dedicated to preventing harm at all staff levels—from the frontline to the corporate level. These HROs promote the reporting of errors and “near misses” without fear of blame or loss of employment.8 In the ED, a culture of safety encourages teamwork, event reporting, communication openness, transparency with feedback and learning from errors, and administrator collaboration for safety.9
In EDs with a strong safety culture, near misses are more likely to be intercepted to reduce patient harm.3 Teamwork training improves communication and reduces errors.10 One such program, Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS), was developed by a joint effort of the US Department of Defense and Agency for Healthcare Research and Quality to promote interprofessional communication between all providers in the hospital. This program provides many tools, including one to obtain attention in difficult situations and one to escalate concerns to focus on an important safety issue.11 One ED’s experience with TeamSTEPPS led it to identify specific steps to ensure continued success after the initial start. To maintain the high level of teamwork and successful communication, this ED recognized a need for continued champions at all staff levels and all new staff members were required to go through the training.12
Another important aspect of a strong safety culture is creating an environment that promotes reporting of adverse events and near misses. The culture should allow a person involved in an adverse event to feel comfortable reporting such events. In one study of 522 “unintended events” at 10 EDs in the Netherlands, nurses reported 85% of events, and resident physicians reported 13% of events. Approximately 83% of reports were filed by a person involved in the event.13 This study highlights EDs that foster a “no blame” environment, where staff members feel comfortable admitting mistakes, and there is no fear of punishment or concern for job loss. When administration supports such reporting, the true safety problems in the ED are identified and can be targeted for improvement.