Neuropsychiatric symptoms of dementia: Monotherapy, or combination therapy?
A cholinesterase inhibitor plus memantine may be more effective than either medication alone.
Evidence for dementia-specific medications
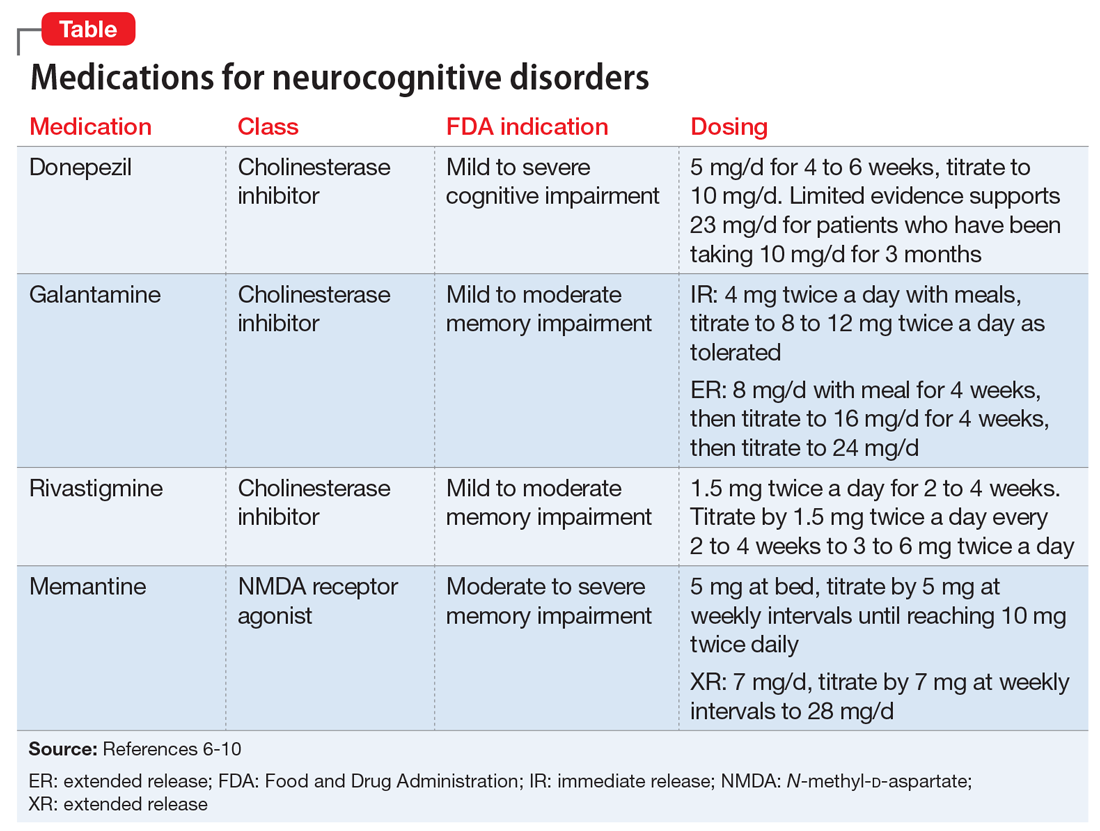
An alternative to the above pharmacologic options is treatment with a cholinesterase inhibitor and/or memantine. Among cholinesterase inhibitors
Few randomized controlled trials (RCTs) of cholinesterase inhibitors or memantine have focused on improvement of NPS as a primary outcome measure, but some RCTs have used treatment of NPS as a secondary outcome.4 Most RCT data for using medications for NPS have come from small studies that lasted 17 days to 28 weeks and had design limitations. Most meta-analyses and review articles exclude trials if they do not evaluate NPS as a primary outcome, and most RCTs have only included NPS as a secondary outcome. We hypothesize that this is because NPS is conceptualized as a psychiatric condition, while dementia is codified as a neurologic condition. The reality is that dementia is a neuropsychiatric condition. This artificial divergence complicates both the evaluation and treatment of patients with dementia, who almost always have NPS. Medication trials focused on the neurologic components for primary outcomes contribute to the confusion and difficulty of building an evidence base around the treatment of NPS in Alzheimer’s disease. Patients with severe NPS are seldom included in RCTs.
A cholinesterase inhibitor, memantine, or both?
In the absence of extended RCTs, attention turns to the opinions of panels of experts examining available data.
The 2012 Fourth Canadian Consensus Conference on the Diagnosis and Treatment of Dementia12 recommended a trial of a cholinesterase inhibitor in most patients with Alzheimer’s disease or Alzheimer’s disease combined with another type of dementia. The panel did not find enough evidence to recommend for or against the use of cholinesterase inhibitors and/or memantine for the treatment of NPS as a primary indication. However, they warned of the risks of discontinuing a cholinesterase inhibitor and suggested a slow taper and monitoring, with consideration of restarting the medication if there is notable functional or behavioral decline.
Continue to: In 2015, the European Neurological Society and the European Federation of Neurological Societies...






