Torsades de Pointes in Severe Alcohol Withdrawal and Cirrhosis: Implications for Risk Stratification and Management
Torsades de pointes (TdP) is a life-threatening ventricular arrhythmia that is associated with both congenital and acquired QT interval prolongation. QT interval prolongation is commonly observed in acute alcohol withdrawal and cirrhotic cardiomyopathy.1-3 In both conditions, there is a positive correlation between the degree of QT interval prolongation and disease severity.4,5 The precise mechanisms of QT interval prolongation in these conditions are not well understood. One hypothesis is that autonomic hyperexcitability results in altered ventricular repolarization and QT interval prolongation. This mechanism of QT prolongation has been found in acute alcohol withdrawal independent of electrolyte abnormalities, use of QT-prolonging medications, and cirrhosis.1,2,6
The authors report the case of a veteran who was hospitalized for acute alcohol withdrawal and decompensated cirrhosis and was found to have a newly prolonged QT interval. On hospital day 3, the patient developed TdP, which required external defibrillation. Despite correction of electrolyte abnormalities, abstinence from alcohol, avoidance of QT-prolonging medications, and exclusion of cardiac ischemia, there was significant and persistent prolongation of the QT interval—ultimately attributed to cirrhotic cardiomyopathy. Acquired QT interval prolongation is common in both acute alcohol withdrawal and cirrhosis.This case highlights the importance of close monitoring of the QT interval and TdP susceptibility in patients being treated for acute alcohol withdrawal, particularly those with cirrhosis.
Case Report
A 66-year-old male veteran with a 35-year history of alcohol dependence presented for alcohol detoxification. He reported having drunk at least 32 ounces of vodka every day of the preceding 5 years and reported having unsuccessfully attempted self-detoxification several times. Prior detoxification efforts were unsuccessful because of intractable nausea and tremulousness. Additional presenting symptoms included lethargy, anorexia, and a fall with transient right-side hemiparesis (findings on magnetic resonance imaging of the head had been normal).
His medical history included type 2 diabetes, tobacco dependence, and macular degeneration. The only medication being taken was glargine 25 units daily. On admission, the patient was afebrile (98.1°F), normotensive (103/77 mm Hg), and oriented to person, place, and time. Examination also revealed a protuberant abdomen with caput medusae, and no shifting dullness or lower extremity edema. The neurologic examination was nonfocal.
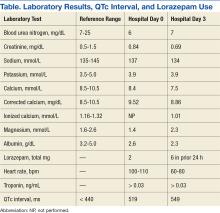
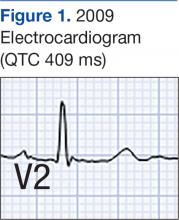
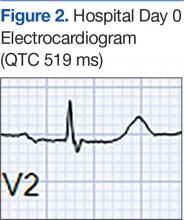
Laboratory test results on admission were significant for elevated serum alcohol level (243.8 mg/dL); elevated levels of aspartate aminotransferase (144 units/L) alanine aminotransferase (25 units/L), and total bilirubin (4.2 mg/L); hypoalbuminemia; normocalemia; hypomagnesemia; normal corrected calcium level; and normal renal function (0.84 mg/dL)(Table). The patient’s admission Child-Pugh score of 10 indicated class C liver disease. Admission electrocardiogram (EKG) revealed normal sinus rhythm, first-degree atrioventricular block, and prolongation of the QTc interval (519 ms). Six years earlier, the patient’s QTc interval had been 409 ms (Figures 1 and 2). As QT interval depends on heart rate, it is most commonly expressed as corrected QT, or QTc, where QTc = QT/(√RR).
Symptom-triggered therapy for alcohol withdrawal was instituted, and the patient’s electrolyte abnormalities were corrected. Telemetry monitoring demonstrated polymorphic ventricular ectopy, including a 6.8-s run of polymorphic ventricular tachycardia and several shorter runs (4-10 beats) of nonsustained ventricular tachycardia, prompting initiation of a low-dose beta blocker. Based on elevated scores on the symptom-triggered scale for alcohol withdrawal, the Clinical Institute Withdrawal Assessement for Alcohol Withdrawal (CIWA), several doses of oral lorazepam were given for withdrawal symptoms.
The patient became increasingly confused, and new-onset nystagmus was noted. These findings raised concern for Wernicke encephalopathy, so the patient was empirically started on IV high-dose thiamine supplementation. The CIWA scores remained high, and there were frequent episodes of ventricular ectopy during the first 2 hospital days. Interval EKG revealed further prolongation of the QTc interval (549 ms) without evidence of cardiac ischemia (Figure 3). Cardiac enzymes were negative, and electrolyte levels were within normal limits.