Sort Out Surgical Cases
Hospitalists often are involved in the care of a surgical patient. Reimbursement for surgical procedures includes payment for pre-, intra-, and post-operative care.
Knowing the billing and coding responsibilities apart from those of the surgeon is imperative for the hospitalist’s accurate charge capture. There are several critical misconceptions in this regard:
- Hospitalists cannot bill for services when involved in a surgical case;
- Surgeons are not responsible for inpatient care if the patient is stable and does not require additional inpatient post-op visits; and
- Modifiers are not required for hospitalist claims unless the hospitalist reports under the same tax identification number as the surgeon.
Determine Global Period
Procedures are categorized as major or minor surgery. A global period is assigned to each procedure code, designating post-operative periods of zero, 10, or 90 days. Physician services during this global period are considered part of the packaged payment and not separately reimbursed.
The global period for any given CPT code can be identified in the Medicare Physician Fee Schedule and accessed at www.cms.hhs.gov/PfsLookup. In addition to zero, 10, and 90 days, services can be noted with:
- XXX, indicating the global period concept does not apply; or
- ZZZ, indicating an “add-on” procedure that must always be reported with the relevant primary procedure code; “add-on” procedures assume the global period of the primary procedure.
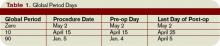
Major surgery routinely is allotted 90-day global periods. Therefore, the surgeon is responsible for the patient and must provide all related care one day prior to the surgery forward thru 90 postoperative days at no additional charge. Minor surgery, including endoscopy, has zero or 10-day postoperative periods, bundling all services on the surgical day only, or the surgical day and the subsequent 10 days, respectively (see Table 1, p. above).
The Surgeon Defined
Any qualified physician able to perform “surgical” services within his scope of practice is considered a “surgeon” for billing purposes. For example, a pulmonologist, or primary care physician, must meet the surgical billing and documentation requirements when performing bronchoscopies or uncomplicated incision-and-drainage services, respectively.
Surgical services easily are identified as any code included in range 20000-69999. This code series includes major, minor, and endoscopic procedures. The “surgeon” and all physicians in the same group practice (i.e., reporting services under the same tax identification number) with the same specialty designation must adhere to the global period billing rules.
Alternately, physicians with different specialty designations in the same group practice (e.g., multispecialty group that reports services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed upon) transfer of care did not occur. Information on physician specialty designations is available at www.highmarkmedicareservices.com/partb/refman/appendix-d.html.