Improving patient outcomes with better care transitions: The role for home health
ABSTRACTPatients, particularly the old and frail, are especially vulnerable at the time of hospital discharge. Fragmentation of care, characterized by miscommunications and lack of follow-up, can lead to oversights in diagnosis and management. The frequent result is avoidable rehospitalization. Amedisys, a home health and hospice organization, created and tested a care transitions initiative for its impact on patients’ quality of life and avoidable rehospitalizations. The initiative was carried out in three academic institutions with 12 months of observation. The results suggested reduced hospital readmissions and a critical role for the home health industry in improving patient outcomes and reducing costs.
Using a care transitions coordinator
Amedisys has placed CTCs in the acute care facilities that it serves. The CTC’s responsibility is to ensure that patients transition safely home from the acute care setting. With fragmentation of care, patients are most vulnerable during the initial few days postdischarge; this is particularly true for the frail elderly. Consequently, the CTC meets with the patient and caregiver as soon as possible upon his or her referral to Amedisys to plan the transition home from the facility and determine the resources needed once home. The CTC becomes the patient’s “touchpoint” for any questions or problems that arise between the time of discharge and the time when an Amedisys nurse visits the patient’s home.
Early engagement and coaching
The CTC uses a proprietary tool, Bridge to Healt0hy Living, to begin the process of early engagement, education, and coaching. This bound notebook is personalized for each patient with the CTC’s name and 24-hour phone contact information. The CTC records the patient’s diagnoses as well as social and economic barriers that may affect the patient’s outcomes. The diagnoses are written in the notebook along with a list of the patient’s medications that describes what each drug is for, its exact dosage, and instructions for taking it.
Coaching focuses on the patient’s diagnoses and capabilities, with discussion of diet and lifestyle needs and identification of “red flags” about each condition. The CTC asks the patient to describe his or her treatment goals and care plan. Ideally, the patient or a family member puts the goals and care plan in writing in the notebook in the patient’s own words; this strategy makes the goals and plan more meaningful and relevant to the patient. The CTC revisits this information at each encounter with the patient and caregiver.
Patient/family and caregiver engagement are crucial to the success of the initiative with frail, older patients.8,9 One 1998 study indicated that patient and caregiver satisfaction with home health services correlated with receiving information from the home health staff regarding medications, equipment and supplies, and self-care; further, the degree of caregiver burden was inversely related to receipt of information from the home health staff.10 The engagement required for the patient and caregiver to record the necessary information in the care transitions tool improves the likelihood of their understanding and adhering to lifestyle, behavioral, and medication recommendations.
At the time of hospital discharge, the CTC arranges the patient’s appointment with the primary care physician and records this in the patient’s notebook. The date and time for the patient’s first home nursing visit is also arranged and recorded so that the patient and caregiver know exactly when to expect that visit.
Medication management
The first home nursing visit typically occurs within 24 hours of hospital discharge. During this visit, the home health nurse reviews the Bridge to Healthy Living tool and uses it to guide care in partnership with the patient, enhancing adherence to the care plan. The nurse reviews the patient’s medications, checks them against the hospital discharge list, and then asks about other medications that might be in a cabinet or the refrigerator that the patient might be taking. At each subsequent visit, the nurse reviews the medication list and adjusts it as indicated if the patient’s physicians have changed any medication. If there has been a medication change, this is communicated by the home health nurse to all physicians caring for the patient.
The initial home nursing visit includes an environmental assessment with observation for hazards that could increase the risk for falls or other injury. The nurse also reinforces coaching on medications, red flags, and dietary or lifestyle issues that was begun by the CTC in the hospital.
Physician engagement
Physician engagement in the transition process is critical to reducing avoidable rehospitalizations. Coleman’s work has emphasized the need for the patient to follow up with his or her primary care physician within 1 week of discharge; but too frequently, the primary care physician is unaware that the patient was admitted to the hospital, and discharge summaries may take weeks to arrive. The care transitions initiative is a relationship-based, physician-led care delivery model in which the CTC serves as the funnel for information-sharing among all providers engaged with the patient. Although the CTC functions as the information manager, a successful transition requires an unprecedented level of cooperation among physicians and other health care providers. Health care is changing; outcomes must improve and costs must decrease. Therefore, this level of cooperation is no longer optional, but has become mandatory.
OUTCOMES
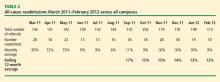
The primary outcome measure in the care transitions initiative was the rate of nonelective rehospitalization related to any cause, recurrence, or exacerbation of the index hospitalization diagnosis-related group, comorbid conditions, or new health problems. The Amedisys care transitions initiative was tested in three large, academic institutions in the northeast and southeast United States for 12 months. The 12-month average readmission rate (as calculated month by month) in the last 6 months of the study decreased from 17% to 12% (Table 2). During this period both patient and physician satisfaction were enhanced, according to internal survey data.
CALL TO ACTION
Americans want to live in their own homes as long as possible. In fact, when elderly Americans are admitted to a hospital, what is actually occurring is that they are being “discharged from their communities.”11 A health care delivery system that provides a true patient-centered approach to care recognizes that this situation often compounds issues of health care costs and quality. Adequate transitional care can provide simpler and more cost-effective options. If a CTC and follow-up care at home had been provided to Mrs. Smith and her daughter upon the first emergency room visit earlier in the year (see “Case study,” page e-S2), Mrs. Smith might have avoided multiple costly readmissions. Each member of the home health industry and its partners should be required to provide a basic set of evidence-based care transition elements to the patients they serve. By coordinating care at the time of discharge, some of the fragmentation that has become embedded in our system might be overcome.