Cardiovascular disease in women: Prevention, symptoms, diagnosis, pathogenesis
ABSTRACTThe significant impact of cardiovascular disease on women is receiving increasing attention, and as a result, we are becoming aware of notable sex differences in the underlying mechanisms, presentation, and response to treatment. This review highlights the importance of continued research focused on women.
KEY POINTS
- Aspirin appears to be less beneficial in women than in men in preventing coronary artery disease.
- Debate continues on the benefit of statins for primary prevention, not only in women but in the population as a whole.
- Hormone therapy is not recommended for cardiovascular disease prevention.
- More women than men who present with acute coronary syndromes have atypical symptoms. Nevertheless, most women who have acute coronary syndromes do have typical symptoms such as chest pain.
- Guidelines continue to recommend exercise stress electrocardiography for symptomatic women at intermediate risk who have a normal resting electrocardiogram.
- Conditions that predominantly affect women include microvascular angina, stress cardiomyopathy, and spontaneous coronary artery dissection.
Spontaneous coronary artery dissection
Spontaneous coronary artery dissection (SCAD) is a rare cause of acute coronary syndrome resulting from dissection of the coronary intimal or medial layer and associated hematoma formation, leading to coronary occlusion.45,46 In a case series of 87 patients, 49% presented with an ST-segment elevation myocardial infarction, and 23% were found to have multivessel SCAD.46
SCAD occurs predominantly in young, healthy women (mean age 30–45 years). Approximately 70% of cases are in women, 30% of whom are in the peripartum period.45 The reasons for the increased risk during pregnancy have not yet been elucidated, but changing sex hormones, increased cardiac output and shear stress, and an increased inflammatory response have been implicated.45
Diagnosing SCAD. Coronary angiography should be performed with extreme caution in patients suspected of having SCAD, given the risk of further dissection of the artery with forceful injections. In certain cases, it may be difficult to detect SCAD on routine angiography if there is no communication between the true and false lumen.
If the suspicion for SCAD is high, intravascular ultrasonography or optical coherence tomography can be used to better evaluate the vessel.45 Although optical coherence tomography has greater spatial resolution, it is more costly and is not as widely used as intravascular ultrasonography in the clinical setting
Managing SCAD. Although conservative management and coronary artery bypass grafting have been shown to cause minimal in-hospital morbidity, percutaneous coronary intervention has been complicated by technical failure in up to 35% of patients in one series.46
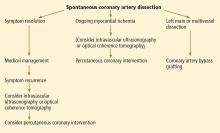
While there is no standardized way to manage these patients, experts currently recommend conservative management with standard therapies for acute coronary syndrome (Figure 4). Although antithrombotic agents can decrease thrombus burden, they must be used with caution, because they also increase the risk of bleeding into the false lumen.
If patients experience recurrent or ongoing ischemia despite conservative management, then revascularization should be considered. Optical coherence tomography or intravascular ultrasonography is recommended to ensure proper stent alignment and positioning.
Coronary artery bypass grafting could be considered in preference to percutaneous coronary intervention, given that the former appears to be safer,46 although this requires further investigation. Some studies have cautioned against using fibrinolytic therapy, based on anecdotal evidence that it may further propagate the dissection,45 although this therapy has been used in other case studies.46
While mortality rates are relatively low (95% survival at 2 years),45 the estimated risk of recurrent SCAD at 10 years is approximately 30%.46
Associated with fibromuscular dysplasia. Of note, a sizeable number of patients with SCAD have been found to have fibromuscular dysplasia. This is a nonatherosclerotic, noninflammatory vascular condition that can affect any vascular bed in the body, although there is a predilection for the renal and carotid arteries (Figure 5).47 Fibromuscular dysplasia also disproportionately affects women and appears to be a concomitant condition in the majority of patients with SCAD.47 Imaging of the carotid and renal arteries of patients with SCAD has revealed a number of cases of fibromuscular dysplasia.46,48 This noted association will likely allow for ongoing research to better understand the pathophysiology of these two conditions.