Sleep disturbances in cancer patients: Underrecognized and undertreated
ABSTRACTSleep-related complaints are extremely common in patients with cancer but often are not recognized, and even if they are, they are seldom treated. Recognizing insomnia in cancer patients is imperative, as appropriate treatment can improve quality of life.
KEY POINTS
- Sleep disturbances, primarily insomnia, profoundly affect all aspects of quality of life.
- Insomnia can be caused or worsened by a number of other conditions, such as pain, fatigue, depression, and anxiety, and these in turn can be worsened by insomnia.
- Cognitive-behavioral therapy is the treatment of choice for chronic insomnia. Underlying problems should be addressed.
- Drugs are often prescribed to help cancer patients sleep but should be used with caution, as there is limited information from clinical trials in this population.
Drug therapy
The focus of therapy should be to treat underlying disorders that may be causing or contributing to insomnia. However, a substantial number of patients may need to be assessed for pharmacotherapy for insomnia.
Sleep problems in the general population are commonly treated with drugs, and most of the recommendations in cancer patients are based on experience in the general population. However, sleep medications should be used cautiously in cancer patients, since to our knowledge there have been no studies of these agents in patients with cancer.
Side effects also need to be considered. For example, sleep medications can profoundly worsen cancer-related fatigue.
Hypnotics are often prescribed for cancer patients.86,87 A study in five major oncology centers showed that about half of the 1,500 patients were prescribed at least one psychotropic drug.86 In this study, hypnotics were the most frequently prescribed drugs, accounting for 48% of total prescriptions, and 44% of the psychotropic prescriptions were written for sleep.
Benzodiazepine receptor agonists such as zaleplon, zolpidem, and eszopiclone can be used for problems with falling asleep and staying asleep.88,89 They are better tolerated than older, long-acting benzodiazepines,90 which can cause alterations in sleep-cycle architecture or rebound insomnia. The earlier agents can also cause adverse effects such as tolerance, drowsiness, and cognitive impairment.
A National Institutes of Health conference stated that benzodiazepine receptor agonists are efficacious in the short-term management of insomnia and that their adverse effects are much less frequent and severe than those of the benzodiazepines or other sedating drugs.84 It also stated that all antidepressants, antihistamines (H1 receptor antagonists), and anti-psychotics have potentially significant adverse effects that raise concerns about their risk-to-benefit ratio and their suitability as treatment for chronic insomnia.
Benzodiazepines are commonly prescribed for insomnia. They increase sleep efficiency, decrease arousals, and increase stage 2 sleep.
Melatonin receptor agonists have been approved by the US Food and Drug Administration for treating insomnia. A recent meta-analysis of eight studies in healthy patients showed improvements in subjective and objective sleep outcomes with the use of ramelteon.91 The dosages primarily used were 4 to 32 mg. However, most of the studies used a dosage of 4 to 8 mg.
Antidepressants. Some of the antidepressants are also used for insomnia, but they can cause daytime fatigue.
Mirtazapine was shown to be effective for insomnia and coexistent mood disorder in cancer patients, but larger trials are needed.92
A recent clinical trial with secondary data analyses evaluated the effect of paroxetine on insomnia, depression, and fatigue in patients with cancer. Paroxetine significantly reduced insomnia in both depressed and nondepressed patients after 2 to 3 weeks of treatment.93
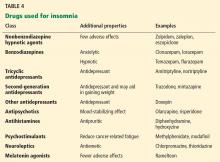
Table 4 summarizes classes of drugs used for insomnia and their additional therapeutic properties.