Hypertensive chronic kidney disease in African Americans: Strategies for improving care
ABSTRACTAfrican Americans have a disproportionate burden of chronic kidney disease (CKD), which tends to have an earlier onset and a more rapid progression in this population. Many of the factors responsible for the rapid progression of CKD in African Americans are detectable by screening and are modifiable with prompt therapy.
KEY POINTS
- To provide optimal care for African Americans, we need to be sensitive to factors that may pose barriers to care, such as poverty, unemployment, lack of insurance, low education level, lack of family support, inaccurate health beliefs, and unhealthy behaviors.
- If we detect CKD earlier, we can better implement strategies to prevent its progression, refer the patient to specialists, and possibly arrange for preemptive kidney transplantation if needed.
- Progression of CKD can be prevented or slowed by controlling blood pressure, proteinuria, and blood glucose. However, CKD progresses in a subset of patients despite evidence-based therapy to target goals.
- African Americans with hypertensive CKD and proteinuria should receive a diuretic, a renin-angiotensin system inhibitor, or both as initial therapy, with a target blood pressure of less than 130/80 mm Hg.
A COMPREHENSIVE APPROACH TO CHRONIC KIDNEY DISEASE CARE
“It is much more important to know what sort of a patient has a disease, than what sort of disease a patient has.”
—William Osler
Many of the risk factors for cardiovascular disease in African Americans are behavioral and modifiable. These include too much salt and fat in the diet, too little physical activity, excessive alcohol intake, and smoking.
Education is key, to identify and communicate the risk attributable to health beliefs and behaviors, particularly in patients with known cardiovascular disease, and to encourage the patient to be proactive in risk-reduction strategies (Table 1). However, effective communication depends on compassion and concern by the health care provider to engender a sense of trust.27 Other health care professionals such as dietitians, pharmacists, and social workers as well as family members can reinforce messages and improve communication with the patient to optimize outcomes.
The International Society on Hypertension in Blacks recommends a blood pressure target of less than 130/80 mm Hg in blacks with elevated blood pressure and target-organ damage. The authors suggest monotherapy with a diuretic or calcium channel blocker if the blood pressure is 10 mm Hg or less above target levels. When blood pressure is more than 15/10 mm Hg above target, two-drug therapy is recommended, either with a calcium channel blocker plus a renin-angiotensin system blocker or, alternatively, in edematous or volume-overload states, with a thiazide diuretic plus a renin-angiotensin system blocker.28,29
The Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease of the National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative recommend starting anti-hypertensive therapy with an ACE inhibitor or an angiotensin receptor blocker for most patients with CKD, regardless of ethnicity, recognizing that many will require combination therapy.30 Evaluation of the response to therapy should include not only checking that the blood pressure is at or below the recommended target of 130/80 mm Hg, but also assessing for complications and monitoring the change in the level of proteinuria, which is a powerful predictor of progression of hypertensive kidney disease in all patients at any given GFR.31
OUR RECOMMENDATIONS
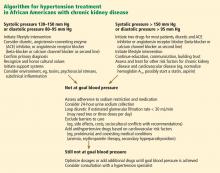
African Americans with hypertension and kidney disease require an aggressive and comprehensive approach to slow the progression of kidney disease and its complications, often necessitating aggressive care of the primary cause and the use of two or more antihypertensive agents to control blood pressure, proteinuria, or both (Figure 1).32
We recommend that the initial evaluation of patients with hypertension include a screening for albuminuria and that the initial therapy for hypertension or proteinuria in all patients with CKD include renin-angiotensin system inhibition with a diuretic, because this combination appears most effective to achieve blood pressure control and to confer additional cardiorenal protection beyond that offered by blood-pressure control alone. Although some studies have reported that African Americans have lower blood-pressure response rates than whites to renin-angiotensin system inhibition, 18 it is nevertheless beneficial for clinical outcomes in this group, especially in the presence of proteinuria, a hallmark of hypertension-related CKD in African Americans. Thus, until more data are available, ethnicity should not be the primary criterion for selecting a given class of antihypertensive therapy, especially in patients with hypertensive nephropathy.
The overall treatment decision should be guided by individual response, coexisting risk factors, and potential cultural and socioeconomic considerations such as cost of medications and insurance coverage, which affect adherence to both pharmacologic and nonpharmacologic interventions.33
Future studies should strive for adequate representation of racial and ethnic minority populations in order to enhance the evidence base for CKD treatment as we move toward using personalized medicine approaches in an increasingly diverse society.34
Acknowledgment: Support for this paper was provided in part by NIH grants RR026138 and MD000182.