Key 2010 publications in behavioral medicine
ABSTRACT
Previous research has demonstrated an association between depression and incident coronary heart disease (CHD); in 2010, well-controlled studies and meta-analyses went beyond depression to include anxiety, anger expression, and negative affect as predictors of incident CHD. Emerging research suggests that positive emotions and resilience (including the ability to self-regulate) offer protection against CHD. New research is elucidating the pathophysiology to explain the effects of emotion and resilience on disease risk; for example, recent work has begun to consider how the relaxation response promotes resilience and found that it induces genomic changes that counter oxidative stress and associated cellular damage.
WHY CONSIDER RESILIENCE?
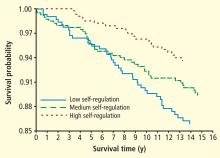
Because the absence of a deficit is not the same as the presence of an asset, greater insight into dysfunction may be gained by explicitly considering what promotes healthy functioning. Ameliorating distress has proven difficult; so, in studying resilience (including the ability to regulate affect), new targets for prevention and intervention may be identified. Although no meta-analysis of resilience factors has been published to date owing to the paucity of data, the studies that have been performed are generally rigorous and have demonstrated consistent findings.
For example, one prospective, well-controlled study of 1,739 men and women demonstrated a protective effect of positive affect (as ascertained by structured interview) against 10-year incident CHD.6 The risk of fatal or nonfatal ischemic heart disease events was reduced by 22% (P = .02) for each 1-point increase in positive affect, even after controlling for depression and negative emotions.
Biology of resilience: Counteracting cellular damage
Genomic changes can be induced by the relaxation response, as evidenced by the differential gene expression profiles of long-term daily practitioners of relaxation (ie, meditation, yoga), short-term (8-week) practitioners of relaxation, and healthy controls.8 Alterations in cellular metabolism, oxidative phosphorylation, and generation of reactive oxygen species that counteract proinflammatory responses, indicative of an adaptive response, were observed in both groups that practiced relaxation.
FUTURE DIRECTIONS
Whether and how the sources and effects of psychosocial stress and response to treatment differ across men and women deserves closer examination. A review by Low et al9 summarizes the current state of knowledge with respect to psychosocial factors and heart disease in women, noting that the sources of stress associated with increased CHD risk differ across men and women; psychosocial risk factors like depression and anxiety appear to increase risk for both men and women; work-related stress has larger effects in men while stress related to relationships and family responsibilities appear to have larger effects in women.
Although responses to psychosocial stress are not clearly different between men and women, intervention targeted at reducing distress is much less effective in reducing the risk of adverse events in women versus men. The mechanism to explain this difference in effectiveness of intervention urgently requires further exploration.
In conducting this work, several factors are important. The best time to intervene to reduce psychosocial distress is unknown; a key consideration will be, what is the best etiologic window for intervention? Perhaps a life-course approach that targets individuals with chronically high levels of emotional distress who also have multiple coronary risk factors, and that enhances their capacity to regulate emotions would prove superior to waiting until late in the disease process.
Another area that may prove fruitful is to consider in more depth the biology of the placebo effect and whether and how it may inform our understanding of resilience.
More generally, considering why interventions seem to influence outcomes so differently across men and women, applying a life course approach to determine the best etiologic window for prevention and intervention strategies, and conducting a more in-depth exploration of the biology of resilience may lead to improved capacity for population-based approaches to reducing the burden of CHD.