New frontiers in cardiovascular behavioral medicine: Comparative effectiveness of exercise and medication in treating depression
ABSTRACT
Exercise, considered a mainstay of cardiac rehabilitation, has been shown to reduce cardiac risk factors such as hyperlipidemia and hypertension. Growing evidence also suggests that exercise has beneficial effects on mental health, which is relevant for cardiac patients because of the prognostic significance of depression in patients with coronary heart disease (CHD). Depression has been associated with increased mortality and nonfatal cardiac events in patients with CHD; it is also associated with worse outcomes in patients who undergo coronary artery bypass graft surgery and those who have heart failure. The standard therapy for depression is pharmacologic treatment, often with second-generation antidepressants such as selective serotonin reuptake inhibitors. Despite their widespread use, antidepressants have only modest effects on depression for many patients compared with placebo controls. Exercise therapy, already an established component of cardiac rehabilitation, has potential efficacy as a treatment for depression in cardiac disease patients. Randomized controlled trials are needed to determine the clinical effects of exercise in this population and to compare the effects of exercise with those of antidepressants.
I am fortunate to be the recipient of the 2010 Bakken Institute Pioneer Award and feel especially honored to have my work recognized in this way. When informed that I was this year’s recipient, it prompted me to reflect on the meaning of the term “pioneer,” and how it related to me.
WHAT IS A PIONEER?
According to Merriam-Webster’s Collegiate Dictionary, a pioneer is one who (a) ventures into unknown or unclaimed territory to settle; and (b) opens up new areas of thought, research, or development. One requirement for any pioneer is that there be a frontier to explore. Thirty years ago, my colleagues and I began our investigations into cardiac rehabilitation (CR), which at the time we considered to be a new frontier for behavioral medicine.1
EXERCISE-BASED CARDIAC REHABILITATION
Historically, patients who suffered an acute myocardial infarction (AMI) were often discouraged from engaging in physical activity; patients were initially prescribed prolonged bed rest and told to avoid strenuous exercise.2 In the early 1950s, armchair therapy was proposed3 as an initial attempt to mobilize patients after a coronary event. Over the years, the value of physical exercise has been increasingly recognized and exercise is now considered to be the cornerstone of CR.4–7 Today, exercise-based CR, involving aerobic exercise supplemented by resistance training, is offered by virtually all CR programs in the United States.8 Proper medical management is also emphasized, along with dietary modification and smoking cessation, but exercise is the centerpiece of treatment.
Exercise has been shown to reduce traditional risk factors such as hypertension and hyperlipidemia,8 attenuate cardiovascular responses to mental stress,9 and reduce myocardial ischemia.10–12 Although no single study has demonstrated definitively that exercise reduces morbidity in patients with coronary heart disease (CHD), pooling data across clinical trials has shown that exercise may reduce risk of fatal CHD events by 25%.13 A recent, comprehensive meta-analysis by Jolliffe et al14 reported a 27% reduction in all-cause mortality and 31% reduction in cardiac mortality.
Not only is exercise considered beneficial for medical outcomes, but is also recognized as an important factor in improved quality of life. Indeed, there has been increased interest in the value of exercise for improving not just physical health, but also mental health.15–17 The mental health benefits of exercise are especially relevant for cardiac patients, as there is a growing literature documenting the importance of mental health, and, in particular the prognostic significance of depression, in patients with CHD.
PSYCHOSOCIAL RISK FACTORS: THE ROLE OF DEPRESSION IN CORONARY HEART DISEASE
There has long been an interest in psychosocial factors that contribute to the development and progression of CHD. More than three decades ago, researchers identified the type A behavior pattern as a risk factor for CHD.18 When subsequent studies failed to confirm the association of type A with adverse health outcomes, researchers turned their attention to other possible psychosocial risk factors, including anger and hostility,19 low social support,20 and most recently, depression.21 Indeed, the most consistent and compelling evidence is that clinical depression or elevated depressive symptoms in the presence of CHD increase the risk of fatal and nonfatal cardiac events and of all-cause mortality.22
Major depressive disorder (MDD) is a common and often chronic condition. Lifetime incidence estimates for MDD are approximately 12% in men and 20% in women.23 In addition, MDD is marked by high rates of relapse, with 22% to 50% of patients suffering recurrent episodes within 6 months after recovery.24 Furthermore, MDD is underrecognized and undertreated in older adults,25 CHD patients, and, especially, minorities.26–28
Cross-sectional studies have documented a higher prevalence of depression in CHD patients than in the general population. Point estimates range from 14% to as high as 47%, with higher rates recorded most often in patients with unstable angina, heart failure (HF), and patients awaiting coronary artery bypass graft (CABG) surgery.29–36
Depression associated with poor outcomes
A number of prospective studies have found that depression is associated with increased risk for mortality or nonfatal cardiac events in a variety of CHD populations. The most compelling evidence for depression as a risk factor has come from studies in Montreal, Canada. Frasure-Smith and colleagues31 assessed the impact of depression in 222 AMI patients, of whom 35 were diagnosed with MDD at the time of hospitalization. There were 12 deaths (six depressed and six nondepressed) over an initial 6-month followup period, representing more than a fivefold increased risk of death for depressed patients compared with nondepressed patients (hazard ratio, 5.7; 95% confidence interval [CI], 4.6 to 6.9). In a subsequent report,36 in which 896 AMI patients were followed for 1 year, the presence of elevated depressive symptoms was associated with more than a threefold increased risk in cardiac mortality after controlling for other multivariate predictors of mortality (odds ratio, 3.29 for women; 3.05 for men).
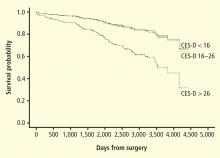
Studies of patients with stable CHD also have reported significant associations between the presence of depression and worse clinical outcomes. For example, Barefoot et al37 assessed 1,250 patients with documented CHD using the Zung self-report depression scale at the time of diagnostic coronary angiography and followed patients for up to 19.4 years. Results showed that patients with moderate to severe depression were at 69% greater risk for cardiac death and 78% greater risk for all-cause death.
Depression and heart failure outcomes
Patients with HF represent a particularly vulnerable group; a meta-analysis of depression in HF patients suggested that one in five patients are clinically depressed (range, 9% to 60%).41 Not only is depression in HF patients associated with worse outcomes,42–46 but recent evidence suggests that worsening of depressive symptoms, independent of clinical status, is related to worse outcomes. Sherwood et al46 demonstrated that increased symptoms of depression, as indicated by higher scores on the Beck Depression Inventory (BDI) over a 1-year interval (BDI change [1-point] hazard ratio, 1.07; 95% CI, 1.02 to 1.12; P = .007), were associated with higher risk of death or cardiovascular hospitalization after controlling for baseline depression (baseline BDI hazard ratio, 1.1; 95% CI, 1.06 to 1.14, P < .001) and established risk factors, including HF etiology, age, ejection fraction, N-terminal pro-B-type natriuretic peptides, and prior hospitalizations. Consequently, strategies to reduce depressive symptoms and prevent the worsening of depression may have important implications for improving cardiac health as well as for enhancing quality of life.