Vagal tone and the inflammatory reflex
ABSTRACT
Inhibition of sympathoexcitatory circuits is influenced by cerebral structures and mediated via vagal mechanisms. Studies of pharmacologic blockade of the prefrontal cortex together with neuroimaging studies support the role of the right hemisphere in parasympathetic control of the heart via its connection with the right vagus nerve. Neural mechanisms also regulate inflammation; vagus nerve activity inhibits macrophage activation and the synthesis of tumor necrosis factor in the reticuloendothelial system through the release of acetylcholine. Data suggest an association between heart rate variability and inflammation that may support the concept of a cholinergic anti-inflammatory pathway.
The neurovisceral integration model of cardiac vagal tone integrates autonomic, attentional, and affective systems into a functional and structural network. This neural network can be indexed by heart rate variability (HRV). High HRV is associated with greater prefrontal inhibitory tone. A lack of inhibition leads to undifferentiated threat responses to environmental challenges.
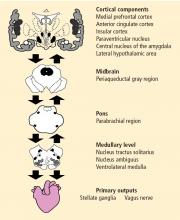
THE CENTRAL AUTONOMIC NETWORK
Activity of the heart permits us to infer activity in this set of neural structures. Excitatory and inhibitory pathways form the connections between the prefrontal cortex and the autonomic output regions in the medullary area, with further connections to heart rate (HR) and HRV.
Central, respiratory, cardiopulmonary, and arterial baroreflex influences on the brainstem signal the sinoatrial node of the heart. Autonomic inputs at the heart have a differential influence. The sympathetic inputs to the sinoatrial node of the heart are relatively slow, such that a burst of sympathetic outflow from the brain produces an effect on the heart several seconds later. In contrast, inputs to the cholinergic or vagal pathway are relatively fast, on the order of milliseconds. The interplay of sympathetic and vagal neural control of the heart produces a complex variability in heart rhythm that characterizes a healthy system.
PARASYMPATHETIC CONTROL AND THE RIGHT VAGUS NERVE
Pharmacologic blockade of prefrontal cortex
The effect of pharmacologic blockade of the prefrontal cortex on HR and HRV was investigated in patients undergoing preoperative evaluation for epilepsy surgery.2 The hypothesis was that inactivation of the prefrontal cortex (using an injection of intracarotid sodium amobarbital) would be associated with an increase in HR and a decrease in vagally mediated HRV.
During 10 minutes of inactivation, an increase in HR was observed in both the left and right hemispheres. HR peaked 3 to 4 minutes postinjection and decreased gradually, returning to preinjection baseline at about 10 minutes. The increase was larger in the right hemisphere, a finding that is consistent with the known neuroanatomy in which the right-sided neural inputs selectively signal the sinoatrial node, and the left-sided inputs signal the atrioventricular node. The pronounced effect on HR in the right hemisphere was related specifically to the vagally mediated (high-frequency) component of HRV. This experiment strongly suggests that cerebral structures tonically inhibit sympathoexcitatory circuits, and that the inhibition is mediated via vagal mechanisms.
Further analysis, in which the subjects were divided into tertiles based on age, revealed disinhibition of brainstem sympathoexcitatory circuits, resulting in an increase in HR of approximately 9 beats per minute in the youngest individuals (mean age, 20 years), but an absence of a laterality effect, which suggests that the prefrontal cortex is not fully developed in this young age group. Disinhibition of sympathoexcitatory circuits as indicated by a HR increase of 11 beats per minute and a right-sided laterality effect occurred in subjects in the second tertile (mean age, 33 years). In the oldest age group (mean age, 45 years), the disinhibition effect on HR was only 3 beats per minute, consistent with the known changes in prefrontal inhibitory tone and prefrontal activity that occur with age.3
Confirmation from neuroimaging studies
Neuroimaging studies support the predominant role of the right hemisphere in the regulation of vagal tone during emotion. Twelve healthy females underwent measurements of cerebral blood flow and the high-frequency component of HRV during two stimulus modalities (film, recall) and six stimulus conditions (happiness, sadness, disgust, and three neutral conditions), for a total of 12 conditions.4 Significant covariation (increased activity associated with increased HRV) was found for four brain areas: the right superior prefrontal cortex, the right dorsal lateral prefrontal cortex, the right parietal cortex, and the left anterior cingulate.