The practical management of gout
ABSTRACT
Gout management requires a comprehensive strategy that considers both acute and chronic aspects of the disease. Acute gout flares should be treated with anti-inflammatory agents as rapidly as possible. The underlying hyperuricemia may be treated with urate-lowering agents initiated at a time appropriate for the individual patient. Successful urate lowering ultimately prevents flares and disease progression and should be started immediately in patients with advanced or tophaceous disease. When urate-lowering therapy is initiated, anti-inflammatory prophylaxis should be used to reduce the risk of flares induced by abrupt changes in urate levels. Regular monitoring of serum urate can ensure therapeutic dosing of urate-lowering agents to achieve levels below 6 mg/dL, which are associated with a reduction in flares and tophi.
KEY POINTS
- A patient’s comorbidities and other medications should guide the choice of anti-inflammatory agent for acute attacks.
- NSAIDs are the treatment of choice for acute gout attacks; colchicine and corticosteroids are alternatives when NSAIDs are contraindicated.
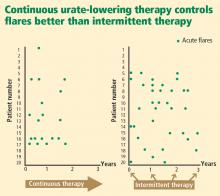
- Urate-lowering therapy to address underyling hyperuricemia is generally a lifelong commitment, as intermittent therapy can lead to recurrent gout flares.
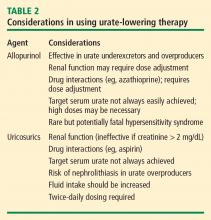
Allopurinol
The rare but potentially fatal hypersensitivity syndrome is a concern with allopurinol. If a rash develops in a patient taking allopurinol, the drug should be discontinued, as rash can be a precursor of severe systemic hypersensitivity.
Renal function must be considered in allopurinol dosing, and treatment should always be initiated at lower doses in patients with renal disease.18 However, recent reports indicate that allopurinol doses can be gradually and safely increased to an effective level that achieves a serum urate concentration of less than 6 mg/dL even in patients with reduced kidney function.19,20
Uricosurics
The uricosuric agent probenecid works by increasing the urinary excretion of urate.10 Probenecid is commonly dosed at 500 mg twice daily, with a maximum daily dose of 2 g, in an attempt to reach the target serum urate level. Probenecid is unlikely to be effective if the patient’s serum creatinine is greater than 2 mg/dL.21
When a uricosuric agent is used, a 24-hour urine urate measurement must be taken to identify and exclude urate overproducers (patients with more than 800 to 1,000 mg of uric acid in a good 24-hour collection), as such patients are at risk for uric acid kidney stones. Additionally, aspirin interferes with probenecid’s effect on the renal tubules. The ideal candidate for uricosuric therapy has good kidney function, is not a urate overproducer, and is willing to drink 8 glasses of water a day to minimize the risk of kidney stones (Table 2).
Evidence supporting urate targets and continuous maintenance of urate reductions
If a serum urate level of less than 6 mg/dL is achieved and maintained, gout flares will be reduced and crystals can be depleted from inside the joint.22–25 Additionally, the size of tophi can be reduced and their recurrence prevented.26–28 Serum urate levels below 4 mg/dL can result in more rapid dissolution of tophi.26
Patient commitment and education are essential
No treatment plan will succeed without the commitment of the patient, so discussion to determine the patient’s willingness to commit to lifetime therapy is warranted. A number of surveys have shown that the rate of continued use of allopurinol after it is initially prescribed is less than 50%.17 If the physician or nurse monitors adherence, however, treatment is more likely to be successful.30
Patients need more education about gout, as education may improve adherence and treatment success. Patient education material is available from the Arthritis Foundation (www.arthritis.org/disease-center.php) and the Gout & Uric Acid Education Society (www.gouteducation.org).
CONCLUSION
A comprehensive treatment strategy is critical to ensure ideal gout therapy. Acute flares should be addressed as rapidly as possible with an anti-inflammatory agent selected on the basis of the patient’s comorbidities and other medications. Most patients require chronic urate-lowering therapy to deplete crystals from joints and prevent flares. Initiation of urate-lowering therapy should be considered early in the disease course, following resolution of the acute attack. Low-dose anti-inflammatory prophylaxis should be initiated when any urate-lowering therapy is started. Regular monitoring of serum urate will ensure effective dosing to achieve a target serum urate level of less than 6 mg/dL. Once urate deposits are depleted, acute flares should cease.