The gout diagnosis
ABSTRACT
Synovial fluid aspiration and analysis is the gold standard for making the diagnosis of gout but is not always performed when indicated in clinical practice. In clinical situations when joint aspiration simply cannot be performed, a presumptive (or clinical) diagnosis of gout may be made in consultation with published recommendations and criteria from expert societies. A thorough patient history and physical examination are critical to a presumptive diagnosis of gout, as is serum urate measurement at the time of an acute attack and at follow-up 2 weeks later.
KEY POINTS
- If the serum urate level was not elevated when measured during an acute attack of arthritis, it will likely be elevated at 2-week follow-up if the patient does indeed have gout.
- Gouty tophi are typically found in the olecranon bursa, whereas rheumatoid nodules are usually located on the extensor surface of the forearm.
- Urate crystals of gout are negatively bifringent and fine and needlelike in shape, whereas the crystals of pseudogout are weakly positively birefringent and rhomboid.
- Gout and septic arthritis can coexist; when the differential diagnosis includes septic arthritis, joint aspiration is required.
- Until criteria for the presumptive diagnosis of gout are validated, clinicians should become familiar with the technique of joint aspiration.
The presence of urate crystals in synovial fluid is the gold standard for diagnosing gout,1 yet clinicians—both primary care physicians and rheumatologists—may not routinely perform synovial fluid analysis even when evaluating a patient who presents with an acute inflammatory arthritis.2 This paper discusses the various reasons why this is so and reviews several important resulting clinical issues: how a presumptive diagnosis of gout is made, when to measure the serum urate level, and special considerations in the differential diagnosis.
SYNOVIAL FLUID ANALYSIS: WHY IS THE GOLD STANDARD NOT MORE ROUTINE?
Occasionally, the aspirated joint does not appear to contain any joint fluid and the clinician may be concerned about the possibility of a “dry tap.” Other possible reasons include lack of experience with synovial fluid aspiration and evaluation, or limited access to the polarizing microscopes used to examine synovial fluid. Time is another factor; in a busy primary care practice, where patients are usually seen approximately every 7 to 11 minutes, there may not be time to aspirate a joint. The urgency of fluid examination is another issue, as synovial fluid must be examined immediately, since the crystals can become smaller, less numerous, and less birefringent with time.4
THE CLINICAL, OR PRESUMPTIVE, DIAGNOSIS
In the appropriate clinical scenario, a presumptive diagnosis of gout can be made on the basis of typical clinical features and the presence of hyperuricemia.1,2
Expert societies offer guidance, but no validation studies to date
Evidence-based recommendations for the diagnosis of gout from the European League Against Rheumatism (EULAR) state that in acute attacks, the rapid development of severe pain, swelling, and tenderness that peaks within 6 to 12 hours, especially with overlying erythema, is highly suggestive of crystal inflammation although not specific for gout.5 These recommendations further state that for typical presentations of gout (such as recurrent podagra [gouty pain in the great toe] with hyperuricemia), a clinical diagnosis alone is reasonably accurate.5
- The presence of urate crystals in joint fluid
- A tophus containing urate crystals
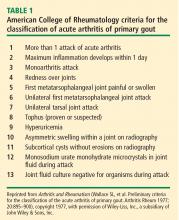
- Fulfillment of 6 or more of the criteria in Table 1.
No subsequent studies have been published on the validity or usefulness of any of these diagnostic criteria.
What must inform the presumptive diagnosis
Both the EULAR recommendations and the ACR criteria state that although the gold standard for diagnosing gout is the presence of urate crystals on synovial fluid analysis, a clinical diagnosis of gout can be made on the basis of certain patient criteria. This clinical, or presumptive, diagnosis of gout should be made based on the following:
- A careful patient and family history, including questions regarding comorbid conditions frequently associated with gout (such as hypertriglyceridemia, diabetes, coronary heart disease, hypertension, and the metabolic syndrome) and whether the patient has had previous similar episodes of acute joint pain and swelling in the absence of trauma
- Thorough identification of all current medications, some of which may be associated with hyperuricemia
- A thorough physical examination.
THE PHYSICAL EXAMINATION FOR GOUT
Examination of patients with a history suggestive of gout should include not only the joints but also the extensor surface of the forearms and feet. When patients are seen for a visit and gout is suspected, they should be instructed to remove their shoes and socks and roll up their sleeves to allow examination for evidence of tophi, which would suggest a past history of gouty arthritis. The ear, knee, and olecranon bursa are other common sites for tophi,3 so patients should also be asked to roll up their pants and sleeves and remove any head coverings.7 In the late stages of gouty arthritis, multiple joints may be involved, which can cause the condition to be confused with other diagnoses such as psoriatic arthritis or erosive osteoarthritis.7
ACUTE PRESENTATIONS OF GOUT
The typical gout presentation is remarkable for very intense pain that often occurs at night when the extremities are colder. Precipitation of urate in the distal extremities can occur when the extremities are horizontal and tend to become cold.8
Approximately 90% of initial gout attacks are monoarticular, leaving only 10% of cases that are oligoarticular or polyarticular.7 If more than one joint is involved, especially if the patient has a family history suggestive of gout or takes a medication that causes hyperuricemia, gout should be considered in the differential diagnosis even if the patient denies having a prior gout attack.
Frequently, patients will call their primary care physician during a gout attack but are not be able to schedule an appointment until after the attack has resolved. When possible, patients should be seen during the attack to confirm whether the attack is due to gout. A diagnosis of gout should not be made over the phone when a patient describes pain in the great toe, as only 50% of initial gout attacks occur in the great toe7 and it is not known what proportion of acute pain episodes in the great toe are attributable to gout. The most common cause of pain in the great toe is osteoarthritis.