Insular Alzheimer disease pathology and the psychometric correlates of mortality
ABSTRACT
Right hemisphere dysfunction is associated with mortality in Alzheimer's disease (AD) and other neurologic conditions. These associations may be mediated by insular pathology, as insular lesions result in demonstrable changes in cardiovascular and autonomic control. AD affects the insulae at a preclinical stage, and insular AD pathology may be present in up to 40% of nondemented septuagenarians and octogenarians. This pathology can affect in vivo cardiac conduction and thereby dispose to cardiac arrhythmias and sudden death. Thus, AD pathology should be considered as a possible explanation for autonomic morbidity and mortality in nondemented elderly persons.
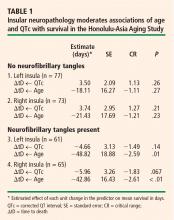
HOLTER MONITOR EVIDENCE
Autopsy studies suggest that as many as 40% of non-demented septuagenarians and octogenarians may have AD pathology that is sufficiently advanced to affect the insular cortex.1 This might explain the high prevalence of supraventricular arrhythmias and longitudinal decreases in heart rate variability among well elderly persons who are free of cardiovascular disease. In fact, unexplained supraventricular arrhythmias are quite common among such individuals. Both tachy-arrhythmias and bradyarrhythmias are common on 24-hour Holter monitor recordings among subjects older than 80 years, and most are unexplained. In a study of the causes of syncope in a large (N = 711) sample of octogenarians, Lipsitz et al confirmed a cardiac etiology in only 21% of cases, whereas 31% of cases were unexplained.6
MORTALITY IN ALZHEIMER DISEASE IS ASSOCIATED WITH RIGHT HEMISPHERE DYSFUNCTION
AD pathology is widely thought to be symmetrically distributed. However, this may not be true of the pre-clinical “limbic” stages of AD.7 Since insular effects on autonomic function are highly lateralized, the side of the brain affected by NFTs may be relevant to effects on cardiac rhythm and, hence, mortality risk.
Interestingly, mortality in AD is specifically associated with right hemisphere metabolic changes by electroencephalography, single-photon emission computed tomography, and positron emission tomography. Mortality can also be specifically associated with tests of constructional praxis. Claus and colleagues found that only the praxis subscore of the Cambridge Cognitive Examination (CAMCOG) was significantly related to survival in patients with early AD (P < .001).8 Its predictive power was based on only two items: copying ability for a spiral and for a three-dimensional house. The effect was independent of age, sex, education, dementia severity, total CAMCOG score, and symptom duration. Similarly, Swan et al found a significant association between performance on the digit symbol substitution test and 5-year mortality among 1,118 subjects (with a mean age of 70.6 years) in the Western Collaborative Group Study.9 In Cox regression analyses, the relative risk for all-cause mortality was 1.44 (95% confidence interval, 1.12 to 1.86) after adjustment for age, education, blood pressure, cancer, cardiovascular/cerebrovascular disease, and smoking.9
RIGHT HEMISPHERE DYSFUNCTION AFFECTS MORTALITY IN OTHER CONDITIONS
The effect of right hemisphere dysfunction on mortality is not limited to AD; it can also be demonstrated in other disorders, including epilepsy, head injury, and stroke.
We have been studying the cognitive correlates of mortality among well elderly septuagenarians and octogenarians living in a single comprehensive care retirement community (CCRC). Once again, visuo-spatial measures have been found to be selectively associated with mortality.10 Clock drawing appears to be the cognitive predictor most strongly correlated with mortality,10 a finding that has been independently replicated in a second CCRC cohort.11 This effect is independent of other cognitive domains, notably executive function.10
SUMMARY
Right hemisphere dysfunction is associated with mortality in AD and other conditions. These associations may be mediated by insular pathology. AD affects the insulae at a preclinical stage, and insular AD pathology may affect as many as 40% of nondemented septuagenarians and octogenarians. This pathology can be shown to affect in vivo cardiac conduction, and may dispose elderly persons to cardiac arrhythmias and sudden death. If so, then AD must be considered a potential cause of cardiac arrhythmia, sudden death, and other autonomic disturbances in nondemented older adults.
Acknowledgments
The author wishes to acknowledge the important cooperation and support received from the Air Force Villages and the Honolulu-Asia Aging Study. This work has been supported by a grant from the National Institute for Neurological Disorders and Stroke (NS45121-01A1).