Clinical hypnosis for reduction of atrial fibrillation after coronary artery bypass graft surgery
ABSTRACT
The belief that postoperative atrial fibrillation (PAF) results from transient autonomic dysfunction suggests that interventions such as clinical hypnosis may reduce the incidence of PAF. To explore this hypothesis, we retrospectively compared outcomes between two groups of patients undergoing coronary artery bypass graft surgery: 50 consecutive patients who received preoperative hypnoidal explanation of the surgical procedure and 50 case-matched historical controls who received no clinical hypnosis. The patients who received hypnosis were significantly less likely to experience an episode of PAF (P = .003) and showed nonsignificant trends toward superior outcomes in terms of length of stay, narcotic use, and total hospital charges. Our findings indicate that prospective randomized trials are warranted to further delineate the potential benefit of clinical hypnosis for prevention of PAF.
Postoperative atrial fibrillation (PAF) is the most common complication of coronary artery bypass graft surgery (CABG), affecting approximately 20% to 40% of patients undergoing this procedure.1 Occurrence of PAF has been associated with prolonged hospital and intensive care unit (ICU) stays, a decline in neurocognitive ability, an increased risk of stroke and transient ischemic attacks, increased surgical mortality, and increased resource utilization and cost.2
The role of the autonomic nervous system in atrial fibrillation (AF) has been studied extensively, but the impact of the autonomic nervous system on PAF has received little attention. Research on the mechanisms of AF has shown imbalance in the autonomic nervous system when measured using heart rate variability. These studies have demonstrated an increase in sympathetic activity approximately 20 minutes prior to the onset of AF, with a shift to parasympathetic activity directly prior to onset. A correlation between mental stress and changes in the autonomic nervous system, as assessed by heart rate variability, has also been shown.3–7
Pharmacologic interventions, including beta-blockers and amiodarone, have been proposed as preventive measures for PAF, but the incidence of PAF remains high.1 Beta-blockade may not be tolerated by patients postoperatively, and there is no consensus on dosing parameters. A meta-analysis on the use of amiodarone in the prevention of PAF was inconclusive,8 and the optimal dosing regimen and incidence of adverse events with amiodarone have not been determined.
There are a small number of studies linking clinical hypnosis to changes in the autonomic nervous system.9 Clinical hypnosis also has been associated with reductions in anxiety and depression before and after surgical procedures.10,11 If PAF is a result of transient autonomic dysfunction, then interventions that alter autonomic tone should influence the incidence and duration of PAF. We report here a retrospective analysis of the impact of clinical hypnosis on the occurrence of PAF in patients undergoing CABG.
METHODOLOGY
Fifty consecutive patients undergoing first-time CABG between October 2004 and May 2005 received preoperative hypnoidal explanation of the surgical procedure as part of their preparation for surgery. A group of 50 case-matched patients who had undergone CABG at the same center between October 2003 and May 2004 were chosen as historical controls.
The treatment group (hypnosis group) and the control group were case-matched for presence of diabetes mellitus, use of beta-adrenergic blocking agents, and use of antiarrhythmic medications. The groups were also matched for various predictors of postoperative PAF, such as age, gender, and coronary artery disease. The patients were all treated by the same surgeon (R.N.), with no significant alterations to surgical or pharmacologic protocols.
The surgeon used indirect Ericksonian techniques during the preoperative explanation of the surgery. Milton Erickson, one of the most prominent hypnotherapists in recent times, used an indirect approach to weave suggestions into the dialogue rather than giving direct commands. This approach encourages active participation and gives the patient a sense of greater control in the hospital environment. The surgeon also instructed patients in self-hypnosis using respiration and imagery.
RESULTS
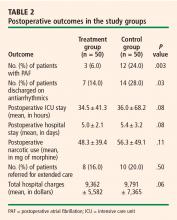
Table 2 presents outcomes in the two study groups. Patients who were treated with clinical hypnosis were less likely to experience PAF: the percentage of patients with one or more episodes of PAF was 6.0% in the treatment group versus 24.0% in the control group (P = .003). Likewise, the percentage of patients who were discharged on amiodarone was 14.0% in the treatment group versus 28.0% in the control group (P = .03).
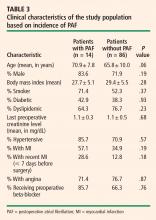
Clinical characteristics were tabulated and compared between the subjects who experienced new-onset PAF and those who did not experience PAF to determine whether there was a covariate responsible for the results observed. With the exception of age, the difference in clinical characteristics between these groups of patients was not statistically significant (using P > .10 as the threshold for significance) (Table 3).