Overview of breast cancer staging and surgical treatment options
ABSTRACT
Following diagnosis of breast cancer, patients undergo assessment for local and systemic treatment. Establishing a relationship and communication with the patient is critical to this assessment, as are history-taking, clinical breast examination, review of imaging studies, and interactive discussion with the patient of treatment options and possible breast reconstruction. Some type of surgical therapy is indicated in virtually all women with breast cancer, generally as the first part of a multicomponent treatment plan. The main goal of surgical therapy is to remove the cancer and accurately define the stage of disease. Surgical options broadly consist of breast conservation therapy, generally followed by radiation therapy, or mastectomy. The surgical procedure also includes assessment of regional lymph nodes for metastasis, either by axillary lymph node dissection or by the less-invasive sentinel lymph node biopsy, for the purpose of cancer staging and guiding adjuvant therapy.
Sentinel node biopsy: A less-invasive alternative
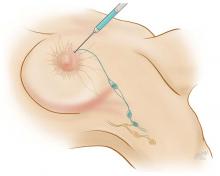
Axillary lymph node dissection has been called into question over the last 15 years due to its invasiveness and the potential morbidity associated with it (including lymphedema and paresthesias). As a result, sentinel lymph node biopsy, a minimally invasive technique for identifying axillary metastasis, was developed to avoid the need for (and risk of complications from) axillary lymph node dissection in patients who have a low probability of axillary metastasis.
Overall, however, it is now accepted that intraoperative lymph node mapping with sentinel lymphadenectomy is an effective and minimally invasive alternative to axillary lymph node dissection for identifying nodes containing metastases.
CONCLUSIONS
Decisions surrounding the choice of breast surgery procedure must be individualized to the patient and her desires and based on comprehensive patient evaluation and thorough patient counseling. Optimal results for the patient—oncologically, psychologically, and in terms of cosmetic outcomes—require consultation and collaboration among general surgeons, medical oncologists, genetic counselors, radiation oncologists, radiologists, and plastic surgeons to clarify the risks and benefits of various intervention options. Striving for this multidisciplinary collaboration will promote optimal patient management and the most favorable clinical outcomes.