Synthetic legal intoxicating drugs: The emerging ‘incense’ and ‘bath salt’ phenomenon
ABSTRACTSynthetic legal intoxicating drugs (SLIDs), such as those commonly contained in products sold over the counter as “bath salts” and “incense,” have risen tremendously in popularity in the past few years. These drugs can have powerful adverse effects, including acute psychosis with delusions, hallucinations, and potentially dangerous, bizarre behavior.
KEY POINTS
- These products are sold under misleading names and deceptive labels to avoid regulation. Although several have recently been banned, many more are waiting to be brought to the market in a similar fashion.
- “Incense” products often contain synthetic cannabinoids; scientific research into their potential long-term effects in humans has been very limited.
- The potential for medical and psychiatric adverse events from synthetic cannabinoids may be heightened because of their full-agonist mechanism of action and because of the variable concentration and unregulated potency of these compounds in incense products.
- Bath salt intoxication, when encountered in the emergency department, may present as a psychiatric disorder or as a range of medical problems including cardiovascular issues, seizures, and hyperthermia.
MEDICAL CONCERNS REGARDING SYNTHETIC STIMULANTS
The medical and psychiatric sequelae that are associated with the use of bath salts have sent an increasing number of people to emergency rooms. The number of bath-salt-related calls to US poison control centers increased dramatically from 303 in 2010 to 4,720 by August 31, 2011. Most of these calls were related to tachycardia, agitation, hallucinations, extreme paranoia, delusions, and elevations in blood pressure.3
A report of 35 cases of people who had used bath salts and who had reported to Michigan emergency rooms between November 13, 2010, and March 31, 2011, indicated that agitation was present in 66%, tachycardia in 63%, delusions and hallucinations in 40%, seizure or tremor in 29%, hypertension in 23%, drowsiness in 23%, paranoia in 20%, and mydriasis in 20%; one patient was dead on arrival. Of the 34 patients who were alive on arrival, 17 (50%) were hospitalized, 15 were released, and 2 left against medical advice. In the patients in this study, 63% had injected the drug, 26% snorted it, and 11% ingested it orally.2 Toxicology results obtained during an autopsy on the one person who died revealed a high level of MDPV, and the coroner ruled that MDPV toxicity was the primary cause of death.2
Though the pharmacokinetic properties of mephedrone are unknown, James et al24 noted that an interesting feature is that its clinical effects seem to persist for more than 24 hours after the last exposure to the drug, which would not be expected based on the rapid elimination of other similar cathinones.
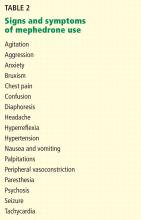
Sympathomimetic toxicity. Many of the symptoms listed in Table 2 are consistent with a sympathomimetic syndrome. In a case series reported by Regan et al,26 most of the 57 patients exhibited cardiovascular findings consistent with sympathomimetic toxicity.
In the study by James et al,24 one of the patients with chest pain had electrocardiographic changes consistent with acute myocardial infarction. Though it is not possible to conclude from a single case that mephedrone poses a risk of myocardial infarction, such a risk has been reported with khat.28 More research is needed to determine whether mephedrone poses a risk of cardiac events when used by people with or without an underlying cardiac condition.
Seizure also seems to be a relatively common feature associated with mephedrone use in case series of emergency room presentations. The US Centers for Disease Control and Prevention l2 reported that of 35 patients who had used bath salts, 40% experienced seizures or “tremors.” A recent case series27 of 15 patients presenting to an emergency department after mephedrone use reported that 20% had experienced seizures. In the study by James et al,24 four patients (3% of the total group) experienced seizures after using mephedrone. It should be noted that, aside from people presenting to emergency rooms, seizures are rarely reported in the wider population of mephedrone users.
Psychotic symptoms are also quite common in users of synthetic stimulants who present to emergency rooms, occurring, as previously stated, in 14% to 40% of cases.2,24
In a small case series, Penders and Gestring29 pointed out some common features in three patients who had used MDPV and had presented with psychosis: sleep problems, inattention, vivid hallucinations of intruders, fearfulness, and inability to remember many of the events surrounding their drug use. The authors concluded that the psychotic syndrome present in their three patients was indicative of a short-term delirium rather than a substance-induced psychosis based on the presence of attention deficits and memory problems. The patients in this series responded well to brief hospitalization and antipsychotic medications.
As with seizure, extreme presentations such as psychosis are infrequently mentioned except in people requiring treatment at a hospital. There are simply no data regarding the prevalence of psychotic symptoms in the larger group of all synthetic stimulant users.
SUSPECT SLID INTOXICATION IN ‘PSYCHIATRIC’ PATIENTS
Despite the temporary ban on the more common substances found in Spice and bath salts, it is premature for the medical community to breath a sigh of relief. Producers of these products are already likely bringing to market new ones containing similar but as yet nonbanned substances. Furthermore, such bans will do little to affect Internet commerce; rather than go to a head shop, consumers will order the products online.
Doctors in urgent care centers, emergency rooms, and on general medical floors should pay close attention to any patient without a known psychiatric history who is acting in a bizarre fashion. Most SLID-intoxicated patients will present with anxiety, agitation, and psychosis. Rather than assume that they are psychiatric patients, one should consider the possibility of SLID intoxication and pay close attention to the possible medical sequelae associated with SLID use, such as elevated blood pressure, tachycardia, and seizure.
Benzodiazepines, especially lorazepam (Ativan), have been the agents most commonly used to treat both agitation and seizures associated with SLID intoxication.
Antipsychotics should be used judiciously because of their propensity to lower the seizure threshold, and patients with synthetic stimulant toxicity are already at increased risk of seizure.
A psychiatric consult should be considered in the event of any suspected toxicity or for any patient whose behavior is difficult to manage.
Restraints may be needed in some circumstances when agitation cannot be controlled with benzodiazepines alone, to ensure safety for the patient as well as that of others in the emergency department.
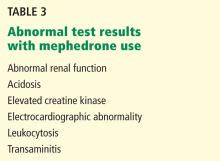
Routine laboratory tests should be part of the workup of patients suspected of being under the influence of SLIDs. These include a complete blood cell count, complete metabolic panel, and urine toxicology (Table 3).23,25 A routine urine toxicology study will likely be negative, but either the patient or collateral information may give you a general idea of what the patient used, in which case the sample could be sent out for special tests for the more common substances found in herbal incense or bath salt products.
Electroencephalography may be indicated if there is any question as to whether the patient may have suffered a seizure. There should be a low threshold to order electrocardiography, especially in the case of synthetic stimulant intoxication.
Serial cardiac enzymes may be warranted if a patient with synthetic-stimulant intoxicated has chest pain.
Education, addiction treatment. Much is unknown about the risk of SLIDs, but given the adverse events reported in the literature, it seems likely that those with underlying cardiac or psychiatric issues may be at higher risk for the most serious drug-related consequences. With regard to synthetic stimulants, Winstock et al20 recommend a harm-reduction approach involving educating patients about avoiding the development of tolerance, not engaging in polydrug use, not injecting, and paying special attention to remaining cool and well hydrated.
Experience shows that once SLID patients get through their acute crisis and are no longer psychotic, they tend to be forthright in divulging what they used to get high. At that point, consideration should be given to consulting an addiction treatment specialist for further evaluation of the patient’s drug use history and for formulation of a treatment plan to help ensure that the patient doesn’t return to using these drugs.