Psychiatric symptoms of dementia: Treatable, but no silver bullet
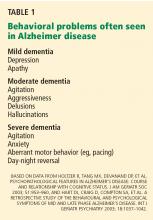
ABSTRACTBehavioral problems are common in dementia and may reduce the quality of life of the patient and disrupt the home life of family members. Families want a pill that can cure the myriad phenotypes of a decaying brain; unfortunately, there is no pharmaceutical silver bullet. This paper reviews the evidence for using different classes of drugs for the behavior symptoms commonly encountered in dementia, focusing on concerns that the primary care physician would have about using these drugs.
KEY POINTS
- No drug specifically addresses wandering, hoarding, or resistance to care, behaviors that are particularly frustrating to caregivers.
- Many drugs are sedating and increase the risk of falling and injury; antipsychotic use is off-label for dementia and carries significant and possibly lethal adverse effects.
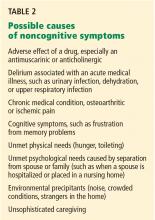
- Managing the behavioral symptoms of dementia requires attention to the environmental and psychosocial context in which they occur, as well as to comorbidities and potential adverse drug effects.
- Evidence for the efficacy of antidepressants for depression in dementia is limited.
Your 84-year-old patient's son is distraught. “I know Mom has dementia, but I don’t understand why she cannot relax. She is busy all night long, taking out the silverware, packing her clothes, and trying to leave the house. Sometimes she tells me that there are little children in the room. These hallucinations scare me, although they do not seem to bother her very much. She keeps me awake; I’m often late to work because I’m up much of the night. I’m afraid I’m going to lose my job; and I don’t want to put Mom into a nursing home. Please give her a medication for this behavior.”
Another of your patients, an 82-year-old man, is admitted to a nursing home after an emergency hospitalization in the geriatric psychiatry unit. His daughter left him alone with her boyfriend one morning while she went to work. Not recognizing him, your patient attacked the young man with a kitchen knife. The police initially arrested your patient and then had him admitted to the psychiatric unit. He is discharged 2 weeks later to the nursing home.
Can anything be done for these patients?
A GROWING PROBLEM
Dementia is a growing problem with the aging of the population. At the time of the 2000 census there were 4.5 million people in the United States with Alzheimer disease, the most common type of dementia,1 and the prevalence is expected to increase to 13.2 million by the year 2050.1
CONSERVATIVE MEASURES ARE THE MAINSTAY OF TREATMENT
As for offending drugs, removing an antimuscarinic or anticholinergic drug may resolve hallucinations; stopping propoxyphene (Darvon) may improve sleep.
No drugs are approved for treating hallucinations, agitation, or other distressing behavior in neurodegenerative diseases such as Alzheimer dementia. Rather, the mainstay of treatment is behavioral and environmental modification.7 In an environment optimized to maximize comfort, reduce stress, and permit safe wandering, behavioral medications may be unnecessary.
Nevertheless, environments are not always optimal, and physicians may offer medications to treat behavioral symptoms to improve quality of life and to let patients keep living in the community.
Below, we discuss the drugs used to treat behavioral problems in dementia, evidence for the efficacy of these drugs, and their potential for adverse effects.
ANTIPSYCHOTIC DRUGS: SMALL BENEFIT, BIG RISK
Although antipsychotic drugs, both typical and atypical, are often used to treat dementia- related behaviors, their beneficial effects are minimal and adverse effects are common.8,9
Aggression has been considered a symptom that might respond to an atypical antipsychotic drug.10 However, the Clinical Antipsychotic Trials of Intervention Effectiveness—Alzheimer’s Disease (CATIE-AD) trial11 found no differences in efficacy between placebo and the atypical antipsychotics olanzapine (Zyprexa), quetiapine (Seroquel), and risperidone (Risperdal) in treating psychosis, aggression, and agitation in dementia. In that study, rates of drug discontinuation due to adverse effects ranged from 5% for placebo to 24% for olanzapine. Overall, 82% of the patients stopped taking their initially assigned medications during the 36-week period of the trial.11
Antipsychotic drugs may cause more adverse effects in patients with Parkinson disease or dementia with Lewy bodies, and medications with the least dopamine D2 receptor blockade are chosen to reduce the impact on the parkinsonism. Patients with movement disorders were excluded from the CATIE-AD study, and data on this topic are very limited. Quetiapine and olanzapine are often used as alternatives to clozapine (Clozaril) for treating psychosis in Parkinson disease and may have a role in dementia with Lewy bodies.12,13
Atypical antipsychotics carry significant risk of illness and even death. The US Food and Drug Administration (FDA) has published advisories about hyperglycemia, cerebrovascular events, and death.14 Returning to the older, “typical” antipsychotics is not a solution either, given their high incidence of extrapyramidal symptoms15 and potentially higher risk of death.16,17
Even if effective, try stopping the drug
Even in the few situations in dementia in which antipsychotics prove efficacious, a trial of dose-reduction and possible discontinuation is a part of the appropriate plan of care. Symptoms such as aggression and delusions may decrease as the underlying dementia progresses.2 A consensus statement on antipsychotic drug use in the elderly18 recommended stopping antipsychotic drugs as follows:
- If given for delirium—discontinue the drug after 1 week
- For agitated dementia—taper within 3 to 6 months to determine the lowest effective maintenance dose
- For psychotic major depression—discontinue after 6 months
- For mania with psychosis—discontinue after 3 months.18
Disorders for which antipsychotics are not recommended are irritability, hostility, generalized anxiety, and insomnia. In contrast with recommendations for dementia-related behaviors, the psychosis of schizophrenia is treated lifelong at the lowest effective dose of medication.