Functional heartburn: An underrecognized cause of PPI-refractory symptoms
Release date: December 1, 2019
Expiration date: November 30, 2020
Estimated time of completion: 1 hour
Click here to start this CME/MOC activity.
ABSTRACT
Functional heartburn—persistent symptoms of esophageal reflux with no objective evidence of gastroesophageal reflux disease (GERD)—is the most common cause of failure of proton pump inhibitor (PPI) therapy, but it is often overlooked by internists and gastroenterologists.
KEY POINTS
- Functional heartburn accounts for more than half of all referrals for PPI-refractory GERD.
- Diagnostic criteria require at least 3 months of symptoms in the 6 months before presentation.
- Results of upper endoscopy with biopsy, esophageal manometry, and esophageal pH monitoring must be normal.
- Patient education is key, with reassurance that the risk of progression to malignancy is low in the absence of Barrett esophagus, and that the condition remits spontaneously in up to 40% of cases.
- Neuromodulators to reduce pain perception are the mainstay of treatment for functional gastrointestinal disorders such as functional heartburn. Cognitive behavioral therapy and hypnotherapy are also used as first-line treatment.
A 44-year-old woman presents with an 8-year history of intermittent heartburn, and in the past year she has been experiencing her symptoms daily. She says the heartburn is constant and is worse immediately after eating spicy or acidic foods. She says she has had no dysphagia, weight loss, or vomiting. Her symptoms have persisted despite taking a histamine (H)2-receptor antagonist twice daily plus a proton pump inhibitor (PPI) before breakfast and dinner for more than 3 months.
She has undergone upper endoscopy 3 times in the past 8 years. Each time, the esophagus was normal with a regular Z-line and normal biopsy results from the proximal and distal esophagus.
The patient believes she has severe gastroesophageal reflux disease (GERD) and asks if she is a candidate for fundoplication surgery.
,HEARTBURN IS A SYMPTOM; GERD IS A CONDITION
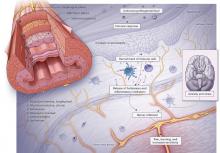
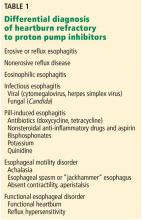
A distinction should be made between heartburn—the symptom of persistent retrosternal burning and discomfort—and gastroesophageal reflux disease—the condition in which reflux of stomach contents causes troublesome symptoms or complications.1 While many clinicians initially diagnose patients who have heartburn as having GERD, there are many other potential causes of their symptoms.
For patients with persistent heartburn, an empiric trial of a once-daily PPI is usually effective, but one-third of patients continue to have heartburn.2,3 The most common cause of this PPI-refractory heartburn is functional heartburn, a functional or hypersensitivity disorder of the esophagus.4
PATHOPHYSIOLOGY IS POORLY UNDERSTOOD
DIAGNOSTIC EVALUATION
Clinicians have several tests available for diagnosing these conditions.
Upper endoscopy
Upper endoscopy is recommended for patients with heartburn that does not respond to a 3-month trial of a PPI.9 Endoscopy is also indicated in any patient who has any of the following “alarm symptoms” that could be due to malignancy or peptic ulcer:
- Dysphagia
- Odynophagia
- Vomiting
- Unexplained weight loss or anemia
- Signs of gastrointestinal bleeding
- Anorexia
- New onset of dyspepsia in a patient over age 60.
During upper endoscopy, the esophagus is evaluated for reflux esophagitis, Barrett esophagus, and other inflammatory disorders such as infectious esophagitis. But even if the esophageal mucosa appears normal, the proximal and distal esophagus should be biopsied to rule out an inflammatory disorder such as eosinophilic or lymphocytic esophagitis.